Dental implants are life changing. For anyone who has lost teeth and is wearing a denture, you probably have already noticed many of the shortcomings with full and partial dentures. For those who have replaced their missing teeth with permanent bridges attached to natural teeth, you may not have as many functional issues compared to dentures, but in the long term you may find that even these bridges have problems and or fail due to decay, gum disease or fracture.
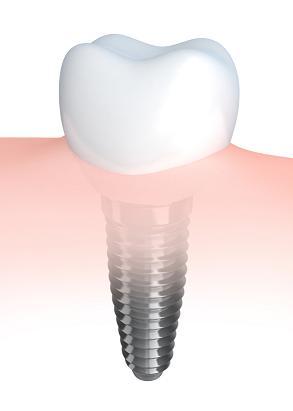
Fortunately dental implants can overcome many of these shortcomings. Dental implants are by far the best method of replacing teeth in the long term when one considers benefits, function and long term success. (Growing new teeth using stem cells may one day be an even better solution but that is at least 15+ years away.) Studies show that traditional crowns and bridges have a 15-20% failure rate within ten years, yet implants have less than 2% failure rate after ten years. If one were to collect longer term data, say 15 to 20 years, the disparity would be even greater.
Unfortunately, there are few things in life that last a lifetime and dental implants are no different. Despite the fact that less than 2% of implants fail, it is not much consolation if you are one of those 2%…as far as you are concerned you have been affected 100%!
So what sorts of things can cause an implant to fail and what can be done to maximize the chance of success? To explain this we have to separate initial or short term failure from long term failure.
Short Term Complications With Dental Implants
Short term failure is best described as those failures that occur before the final teeth are made. It could be immediately following the surgery , during the first few months of healing or even a year later.
1. Infection and Poor Healing
Placing an implant is a surgical procedure. Provided the dentist follows aseptic/sterile surgical techniques and precautions the chance of infection is extremely low, even when we consider we are working within the mouth which is full of bacteria. Patients are generally covered with antibiotics as an added precaution. Discomfort following surgery is usually mild to moderate and lasts for 1-4 days on average, and of course depends on the specific procedure being done. Make sure to ask your dentist what is a normal expectation for yourself.
In over 20 years of placing implants I have only seen two immediate infections (within one to two weeks of surgery) and in both cases it was a result of poor compliance and not following instructions on behalf of the patient. In some cases an infection may develop one month or more following surgery but before the implant is fully integrated (healed). If an infection does occur it is usually because of the presence of an existing problem or infection in a tooth or area adjacent to the surgical site. If caught early in some cases it can be dealt with and the surgery can still be successful.
2. Medical Condition Affecting Healing
Generally speaking, if you have lost teeth, you are a potential candidate for dental implant surgery. However, there are certain conditions and diseases that can affect whether dental implants are right for you – this is where the importance of a proper medical assessment comes in.
Conditions such as cancer, radiation to the jaws, alcoholism, uncontrolled gum disease or diabetes, smoking, certain medications and various other ailments can affect your bodies ability to heal and whether dental implants will fuse to your bone. These are not necessarily absolute contraindications, but steps may need to be taken to ensure that you will heal properly. Your dental surgeon should be taking a thorough medical history and make sure he/she is fully aware of any ailments as well as any medication you’re currently taking to avoid any unnecessary complications.
3. Surgical Technique
A skilled dental surgeon will know the osseo-integration process (how the dental implant anchors to the jaw bone) and be skilled in proper surgical techniques. In those cases healing is often very comfortable and uneventful. If not, the site is more prone to swelling, pain, infection and possible failure of the implant. This becomes more critical if the area is slightly deficient in bone volume or is very dense….overheating of the bone will cause necrosis (bone death) and the implant will likely fail to integrate.
4. Micromovement of the Dental Implant
Dental implants must remain immobile for a long enough period to allow osseo-integration to occur. The analogy I give my patients is similar to when we break a bone in our arm or leg. The fracture is immobilized by use of a cast because if there is movement the bony fracture will not heal. Implants are very similar.
Dental implants take a full 16-17 weeks to fully heal and that is based on a “sigma” of bone…the sigma is the time required for bone to go through a process of remodelling and mineralization. this time frame is constant from person to person, regardless of age or ethnicity.
If there is movement of the implant during the first 8-12 weeks the implant will not become stable because the bone will not grow against the side of the implant. You will get soft tissue ingrowth instead and the resulting implant will be loose and possibly painful.
This is very important for dentists who offer “immediate teeth” or “immediate implants”. In some cases we can place a tooth immediately onto an implant but we have to take steps to ensure that the forces and function on that implant are minimal. That could mean making the tooth shorter so that the food does not press on the tooth, eating a soft or liquid diet for ~2-3 months and/or splinting the tooth to other implants or natural teeth.
Immediate teeth are a wonderful way to have implants especially when it is a front tooth but you need to aware that it does or can pose an increased risk of failure. One final comment…your “bite”…how your teeth fit together…may make it possible or impossible to provide immediate teeth.
5. Lack of Bone
For an implant to be successful, it ideally needs to have bone grow around it on all sides. If the bone is deficient in height or width, steps need to be taken to ensure that bone will indeed grow against the implant.
If you have been missing a tooth for a long time, you will likely have lost some bone volume in that area. We can increase the volume of bone with various techniques. In some cases it has to be done as a separate step, and in other cases it can be done at the same time that the implant is placed.
Your implant dentist should be well skilled in being able to either grow bone via a bone graft or manipulate the site in a way that bone will fill the site. If there is a lack of bone volume and a dental implant is placed without correcting these deficiencies, your implant will likely fail.
Keep in mind that there is a very wide range of skills and techniques among implant surgeons. I have had many patients come to me after they have been told that “they don’t have enough bone and that they can never have an implant(s)”. What a wonderful experience it is for me to see the joy on their face when I tell them that it can be done…and an even greater joy when the final teeth are placed and the work is all said and done!!
6. Not Following Doctor’s Instructions
The post-op instructions are usually fairly straight forward and simple. Keep heavy physical activity to a minimum (usually for a few days), keep the surgical site clean, avoid eating certain foods if instructed to do so, and take your medications as recommended. There may be other specific recommendations that are given to you depending on the surgery being performed or your particular circumstances.
I have had patients do wonderfully the first couple of days and assume that they just happen to be a very fast healer so they carry on with their normal activities….in some cases things they were specifically told not to do…such as swimming, heavy cardio or exercise, eating certain foods etc. Then they begin to experience increased discomfort, swelling and or other complications and soon realize I was serious about the instructions. Keep in mind some medications that we prescribe help to reduce the usual post op problems people expect, and if they begin to overdo things too early they may have a more difficult time healing.
Long-Term Complications With Dental Implants
1. Failure to keep the area clean and maintained
So you finally have your dental implants and your final teeth are in place and now you’re ready to bite into crisp apples and smile bigger than ever before.
Now before you go riding off into the sunset with your new pearly white(s), it’s very important you maintain these new teeth and implants. Although I mentioned in previous blogs that implants are not prone to the same problems we see with natural teeth such as fracture decay and in infections they do require maintenance. I have treated patients who lost their teeth due to long term neglect and lack of care…sometimes these same people still seem to forget to brush their teeth now that they have implants!
If you have dental implants, you have made a major investment in your dental health. It needs to be maintained with simple brushing, flossing and a regular checkup with your general dentist and/or implant dentist.
If you get excessive food or bacterial plaque around an implant and do not clean it regularly it will cause inflammation in the gums which can lead to bone loss, infection and problems and/or even loss of the implant.
For some other reasons I will mention below it is very important to have your teeth checked regularly. I see and treat many patients who have their own “family” dentist and they come to see me for implant treatment only. Even in those situation where I know they are being seen by their own general dentist, I will have them come back for a follow up after one month, one year and then every 3-5 years just to make sure that everything is Ok.
2. Too much stress and forces on the implants
Once an implant has integrated with the bone it is extremely solid…it feels much like a “nail in concrete”. Unfortunately bone is not concrete. If there is excessive stress on a dental implant physiologically the bone will be lost. This may create a periodontal (gum) pocket which in turn will then allow unhealthy bacteria to grow and colonize….this sets up a cascade of event whereby more bone can be lost, infection set in and the implant can eventually be lost.
One of the best ways to prevent this is at the beginning..at the treatment planning stage. Although we are working on teeth, people and human bodies…. a lot of what we do has to do with engineering. If we do not place enough implants, if the implants are too small, too short or on too much of an angle the stress on the implant(s) can be excessive. In these cases your implants may do very well for the first five or so years but then you may begin to see bone loss and failure occurring.
This is why it is very important to be aware of certain treatment proposals that suggest using fewer dental implants or mini implants. There are implant companies out there whose prime directive is to sell more implants and to make the procedure appear simple so that any dentist can place them. I am not saying that fewer dental implants, mini implants or simple procedures are never successful in the long term. But if the forces on the teeth, type of teeth, bone quality, volume and other factors are not considered in the treatment planning you may have an unpleasant surprise as there is a much greater chance of long term failure.
About two years ago I had a patient come to see me as she was having pain with her upper implants. She had four implants placed and these were supporting a set of permanent teeth…the surgeries went well and she healed fine. The final teeth were placed just one and a half years prior to her seeing me. By the time she came into our office three of the four implants were failing and had infection around them, and this infection had caused further bone loss! There was only one implant that had some bone support but it was clear it was already beginning to fail. Once that failed the entire teeth would fall out. From my determination, she did not have enough implant support for the type and number of teeth being replaced and this caused too much stress on the bone. I explained some other options that would have been better and more successful in the long term and she said that someone else had told her something very similar. Basically she went with a less expensive treatment plan to save some costs..unfortunately she spent thousands (and thousands) of dollars and I don’t think she was able to recover any of the costs that she had spent. She will end up spending way more now to fix the damage done and then to restore her mouth more ideally.
3. Less than ideal placement or treatment planning
In some cases patients have had dental implants placed very successfully and have healed very well, only to find that when the teeth are to be made the implants cannot be used. In some cases it is because the implants are not in the right location or angle or the esthetics of the situation will not allow the implant to be useful.
This generally comes about from a lack of planning. The dental surgeon who is placing your dental implants should know exactly what type of teeth you will eventually have because that will determine exactly where, how many and at what angle the implants need to be placed. Therefore your implant treatment needs to start not with a surgeon, but with the dentist who will be providing in the final teeth. In some cases (such as our office) the implant dentist will provide both the surgical and prosthetic(teeth) phases of your dental implants. However, some dentists only provide the prosthetics, and some only provide the surgery. That can also work provided that the two of them communicate and that the treatment planning is done by the prosthetic dentist first…because (as described above) the type of teeth being placed will determine the type of surgery required.
Not to sound so pessimistic but I have had some patients come to see me to have teeth made after having the implants placed but with no prior consultation with myself or a prosthetic dentist. In some cases those implants were not restorable and had to be removed because of esthetic, health or functional concerns.
The Good News About Dental Implants!
While finding a skilled and qualified dentist(s) you can trust and feel comfortable with are important, the success or failure of dental implants also depends on the patient. By working together, you’ll help minimize any potential risks and before you know it, you’ll be read to take a big bite of life.
Despite the pessimistic outlook that you may derive after reading the above complications, dental implants are still the most successful and least problematic method of replacing your teeth. In my opinion, probably the biggest problem is that dental implants are often the most expensive option compared to traditional dentures and bridges. Therefore if you do have complications the potential loss of your investment can be huge. Make sure to ask your dentist(s) what sort of life expectancy is reasonable, and what is their policy regarding “failures.” I have many patients in the office who have had their implants for 15+ years with no issues, and several with implants for 25-37+ years, also with minimal to no issues. (I’ve only been placing and restoring implants for ~25 years so I cannot take credit for some of these patients…but I mention it to illustrate just how long they can last and endure)
If you have any questions, issues or problems you can always call, e mail us or even come in for a consult. We are here to help!

















219 thoughts on “Complications With Dental Implants (And How To Overcome Them)”
Another reason for implant failure is the dentist who places the crown on the implant/abutment. I had a toxic reaction and was extremely sick,in and out of the hospital for months, before I figured out that too much cement toxins got into my blood stream and was caught underneath my gums. I had oral surgery to remove the excess cement, but slowly, the implant eventually failed. It is SO important to have a good dentist that is used to dealing with implants, and places the crown correctly.
Hello Diane,
Thank you for your comment.
Definitely, excess cement around any crown, be it an implant or even a natural tooth, will create a site for oral bacteria to collect and typically cause localized inflammation and potential bone loss.
I would say it is rare that this local problem would spread to the blood/entire body but at the same time I’m not ruling it out altogether.
I would say that really depends on a combination of factors such as your immune system as well as the degree of infection/inflammation.
Dental implants are different from natural teeth, in that depending on how the abutment is made, removing excess cement can be difficult in terms of visualization and access.
The good news is that it is a well-understood problem and the implant industry as a whole has educated dentists on how to avoid this type of problem.
Sincerely,
Dr. Balogh
I have been told I may have cement caught in my gum around my 3 yr old implant, since I am having pain around the tooth with brushing and flossing. I have some pockets around the tooth that when probed, reveal a creamy substance with a distinctive odor, also noticeable with flossing. I was put on 10days of antibiotics and used tiny tapered pick brushes to clean and probe the pockets around the tooth, and rinsing with 3% peroxide mouth wash . After 10 days, problem persists. Continue to have creamy drainage in pockets. Would it be useful to culture the creamy substance? Try a different antibiotis( I had 10days of amoxicillin). Recent hip revision, but other wise healthy 67 yr old. Tooth X-ray does not show bone loss, infection. Tooth feels stable. Only option in front of me is flap surgery to check for cement. What do you recommend?
Hello Kathy
Most likely the creamy substance is pus…infection. This is quite common especially if cement has been trapped under the gum tissue…the cement becomes a place for bacteria to grow an hide. Re the xray…sometimes they can be deceiving in that traditional films are 2 dimensional and may not show what is truly happening around the implant. A 3D ct scan of the area would be best. Most importantly ou do not want to leave it for too long otherwise you will likely lose bone and that can be more difficult to stop/correct. the first thing (besides a ct) would be to remove the crown (if possible) and clean and check the area. YOu could try using a waterpick daily in the area to flush the area with an antibacterial solution (salt water, antibacterial mouthwash). Failing all these these things the area may need to be exposed surgically to truly see what it causing the infection.
Sincerely
dr balogh
I had a tooth extraction with a bone graft and it seemed by bone inside my mouth grew and it hurts like crazy. I’ve been told I need to see a neurologist but honestly I am not sure what is wrong… the jaw hurts, upper teeth hurt, sometimes my ears hurt. I have a temporary mouth guard because I grind my teeth at night. I need an implant but my gums hurt so much and I’m having so many temple and eye headaches and specialists say I heals nicely but I’m still in pain everyday.
Hello Jacqueline: Many of your symptoms can be related to bite and grinding (parafunctional) habits. IT could certainly be a neurological issue but until some of the obvious and more common issues are eliminated it will be difficult to say for sure. Sincerely, Dr Balogh
I had a tooth pulled and bone graft last week. I had the stitches removed today. Is it normal for me to still be feeling a good bit of pressure and a little pain at the site of the graft?
Yes…but should be getting better every 1-2 days….if anything feels like it is getting worse contact your dentist right away.
Sincerely
Dr Balogh
I had front tooth implant,next to implant they put fake front tooth,next to implant added fake tooth ,having pain and gum problems still been 1 year front tooth next to implant sliding down
Hello Linda,
Thank you for your comment.
Placing a single implant in the front area with a false tooth attached to it should not be an issue (we call it a cantilever bridge).
However, that really depends on the strength of the tooth/implant and the bite forces on the crowns.
The gum problems may be related to the ability to clean the area and/or possibly bacteria collecting on the surface of the implant if some of the bone has remodeled.
Regarding your tooth “sliding down” after one year it is really difficult to comment without a better understanding or visualization of the area.
Definitely, the gums around an implant (or any tooth for that matter) should not bleed, be sore, inflamed, have any bad odors or pus coming from the area.
It sounds like you do have at least one of these symptoms so it is wise to have it checked to determine the cause and have it rectified.
Sincerely,
Dr. Balogh
Hi I have gone through the first process (the screw in my mouth) but it isn’t healing well I have pain radiating from my ear to my jaw (some sinus problems too) as well as a headache and some swelling around the tooth area. I’ve taken antibiotics. Not doing well. Any suggestions? It’s been almost 4 weeks
Ty!
Hello Denise,
Thank you so much for your comment.
I am sorry to hear about your discomfort.
It definitely is not normal and if antibiotics did not clear it up with 72 hours there is either something else going on or the area has bacteria resistant to the antibiotic.
Without knowing more or seeing the area for myself it is difficult to say.
You may need to have the implants removed if a problem is suspected around them.
Definitely go back to your surgeon and give him/her the full details and history of your symptoms.
All the best!
Sincerely,
Dr Balogh
Dear Dr. Balogh, I’m thinking of getting full mouth implants. First, I’d like to know what is the best crown material that can be used and using titanium instead of titanium alloy for the posts. My concern is using the best material possible, how much will it cost, and who in the South Florida area is the best oral surgeon who can “do it all” in his or her facility. Please advise me, thank you. Madeline Lepore
Hello Madeline,
Thank you for your comment.
A good source to find a dentist who is qualified would be to go to either the http://www.aboi.org or http://www.aaid.com websites.
They have lists of doctors in each state that have passed certain qualifications and accreditations. Certainly these are not the only accrediting organizations, and no doubt there are some dentists/surgeons who have excellent experience and track records but have not taken the time required (it is an onerous task).
However, beyond these, your best method of discernment would probably be word of mouth, their past patients and your own sense of comfort and confidence once you have met them.
For a single crown itself, zirconia crowns are right now the strongest type of porcelain, however, that does not mean other materials are substandard.
We have to look at the needs of each individual from a functional, aesthetic, longevity and practical standpoint. Once your dentist has an overall plan he or she can also discuss the various materials.
Regarding costs, for a single arch of permanent teeth expect costs anywhere from $25-50,000 per arch…I know that is a huge range but then so much depends on whether there is any need for bone grafting, the number of implants placed as well as the type of teeth being inserted.
Sincerely,
Dr. Balogh
Today is 6/28/17: I had 2 mini implants and a wisdom tooth removed, using Ativan and nitrous oxide gas on March 2nd.
On May 24, I had 3 traditional implants w abutments. I use oil pulling w organic coconut oil 20 min. 3 X’s a day. Everything is healing. This surgery took 4 hrs w gas and Ativan.
I gave been hoarse, down to a whisper, fir 14 days now w a sinus infection. Saw my regular doc yesterday. Z pac and steroids.
Can the hoarsness and sinus come from the gas for prolonged period. I’m seeing a very qualified oral, maxillary surgeon.
Debbie
Hello Debbie,
Thank you for your comment.
It would be quite a different situation if you had had general anesthetic.
Anesthetic can cause irritation because you often need to have a tube placed into your airway.
Since you only had nitrous oxide, I don’t feel your symptoms are due to the gas.
Sincerely,
Dr. Balogh
I have had final stage of implants,
Teeth have been fitted.
I am struggling to eat as the alignment doesn’t feel right.
My tooth which is implanted is rubbing on my bottom tooth.
When I chew my back teeth don’t touch.
What can I I?
I feel the tooth is slightly too long.
Can it be shortened whilst it’s attached?
Any advice will be gratefully received.
Hello Charli,
Thank you for your comment.
I recommend that you go back to see the dentist that made your teeth. It sounds like the bite on your new teeth needs adjustment.
Your dentist should easily be able to make the appropriate changes. The teeth can often be adjusted without having to remove them.
Sincerely,
Dr. Balogh
I had 3 implants placed almost 3 months ago in Mexico(which was a huge mistake. I am having a lot of pain from all 3 sites although sometimes they tend to rotate on which site is hurting more. They were placed so I could attach my lower dentures to the implants. I’m really worried there is something wrong because of the pain. It usually runs about a 5 or 6 out of ten and effects my ability to chew. They have not yet even been put to use. I can’t return to the dentist who did the implants for a follow-up. What sbould i do? What type of doctor/dentist should I try to see to get some help if that’s what you think should happen? Thank you.
Hello Corinne,
Thank you for your comment.
I am sorry to say but something is definitely wrong. You should have had minimal discomfort (1-3 out of ten) for the first 2-3 days and then nothing afterward. It sounds like at least one of the implants has failed to integrate or heal properly.
The best thing to do is to find a local dentist. Preferably one that is familiar in placing implants. Have the area x-rayed and evaluated clinically.
It may be a simple matter of removing the failing implant(s), allowing the area to heal and then possibly replacing it after 2-3 months.
Sincerely,
Dr. Balogh
Hello
I lost my both front upper incisors in an accident when I was a kid ( 10yrs). Now I want to get dental implants. My current age is 21 yrs. There is a gap of 11 yrs. Therefore the area is much lesser than needed. Did I loose part of my jaw bone?. Am I am eligible for getting implants? If yes then how many implants are needed to fix in the bone? One or two? What precautions do I have to take? Also, I am a chain smoker. And I am allergic to nothing.
Hello Khan,
Thank you for your comment.
You probably have experienced partial bone loss in the jaw. This is either from the initial accident or from atrophy due to the many years without the teeth. The bone, however, can usually be built back to close to its original volume.
But you would need to see an implant dentist, to have the area evaluated first. Once the bone is rebuilt, you will likely need two implants, one for each missing tooth. In this area, it usually does not work as well with a single implant to replace both teeth.
Your smoking will make the surgery riskier. It doesn’t mean that it won’t or can’t be successful, but the chances for revisions or results less than expected are greater.
Different implant dentists will have different opinions. In some parts of the world, many people still smoke quite heavily and the dentists in those areas still manage to treat people successfully.
If I were the one doing the surgery I would ask for you to cut down as much as possible for the first 3-5 days, and to consider wearing a nicotine patch.
Sincerely
Dr Balogh
Dear Dr Balogh
I have had my 3 implants at the front of my mouth since the year 2000 and I have been very very pleased with them and have looked after them well. I did have a lot of bone loss intiially (before the implants ) as I lost my front teeth in 1973, so had 27 years with initially a bridge and the dentures (Ugh) I now have an infection above my implants and am due surgery in October – what are your thoughts on using Bovine bone to replace the lost bone (initially due to time and now infection). I am on Antibiotics and mouthwash until Surgery. I would appreciate your thoughts as you talk a lot of sense. Thanks Lynn
Hello, Lynn
Thank you for your comment.
My apologies if my response to your question is too late.
In my experience, there is no problem with using bovine bone. It will work well in the majority of cases and should work well for you.
The “gold standard” has traditionally been to use ones’own bone, however in many cases that means bone volume is limited. (Unless we harvest from the hip, which is much more invasive).
Other materials involve using human donor bone, coral (which is essentially another type of animal) and synthetic bone. The synthetics are very limited in their ability to grow bone.
I could speak or type for an entire day on the pros and cons of the different materials.
Some of the most important factors in growing bone is blood supply. A clean site and isolation /closure of the site to keep the oral environment and bacteria out is ideal.
The technique your dentist uses is sometimes more important than the material used.
If you notice excessive pain at the site or any changes/swelling in your gums, contact your dentist immediately.
Your body could be rejecting the material.
Hopefully this helps and sorry again for responding so late.
Sincerely,
Dr Balogh
I have a front tooth implant and I just had my crown placed about a week ago. I experienced pain through all of my top teeth like I’d had braces tightened. I figured this was due to perhaps some shifting of my teeth while my tooth was out. However, I now have quite a bit of pressure/pain in my hard palate where the implant is screwed into the bone. I am a professional singer and it hurts every time I sing. My oral surgeon is taking a wait and see attitude. Is it normal to have pain in the palate after the crown has been placed?
Hello, Lori
Thank you for your comment.
My apologies for this late response. By now I hope that your pain and discomfort has subsided.
It is not unusual to feel some pressure on the adjacent teeth or tissues when a crown is placed. However, that pressure should ease off within a few minutes to an hour.
If it persists then something either needs to be adjusted or something may be wrong. There could be several things in this category, but most often it is not too serious.
Let your dentist know that your pain has gone on for too long if this has not already been resolved.
I hope this helped to answer your question.
Sincerely,
Dr Balogh
I had 6 upper frontal implants done. Horrible procedure although highly recommended and qualified dental surgeon. Teeth feel too tight. Even under sedation I could hear discussion of “wrong size”. Lots of cracking noises as he tightened stuff. Post surgery pain worst, but I tolerated it. However all sorts of skeletal pain have emerged from skull to toe literally. Yawning, chewing, swallowing everything difficult. Biting inner left cheek. Bottom teeth crushed during procedure so flossing impossible. Huskiness, throat problems. I’m going back for first follow up. How should I open the discussion, what’s reasonable to expect?
Hello Teresa
Thank you for your comment.
I think you have to separate two issues at play here. The surgery and post-surgery pain from the teeth and your prosthetics.
Certainly following a surgery, depending on what was done, there will be some post-operative discomfort.
However, once that has healed, you really should not have any further symptoms like the ones you describe:
“skeletal pain – Yawning, chewing, swallowing everything difficult. Biting inner left cheek”
These issues are more likely related to your teeth and your bite.
Ideally, the final tooth imprint, type, location of the teeth and your bite should have been determined before any surgery.
This would then dictate where the implants need to go, how many and whether there is enough bone in the area. This helps to minimize prosthetic issues when the teeth are finally done.
Definitely, bring up your list of concerns with your dentist right away. Some of these issues such as cheek biting and chewing can often be fixed with a simple adjustment.
The yawning and chewing are a little harder to discern without more information but at least some of these problems can be fixed almost right away.
I hope that helped to answer your question.
Sincerely,
Dr Balogh
Hello Dr. Balogh,
Thank you for all the helpful information. Just yesterday I had to have my lower molar implant removed because it failed. I have two endodontists attending (I began the process in one part of town and moved 40 min. out to another so needed another endodontist to complete the work.) Neither could find anything wrong and were surprised it had failed. In your experience, can an implant work after one has failed? I worry if I go through all this again it may just fail? Have you found a high success rate after a failed implant?
Thanks!
Bridget
Hello, Bridget
Thank you for your comment.
Yes definitely, you can have an implant fail more than once and still have it be successful. I know this first hand because it has happened to me! (In that case, there was an infection in the tooth beside the site that was asymptomatic and no signs clinically or radiographically. Once identified and treated, the next implant worked fine and has been there for over 10 years.)
The most important point is for your dentist to try to determine what caused the first implant to fail. This is the best way to avoid a repeat occurrence. Sometimes it is obvious, other times it’s not as easy to identify.
But there is no need to worry. Some mistakenly think that their body has rejected the material and that they cannot have implants. This is usually untrue and the issue is either local, physical or surgical protocol factors that cause implant failure.
I hope that helped to answer your question.
Sincerely,
Dr Balogh
My implantologist in Costa Rica must have made my post too short because my crown will not stay on unless my dentist here in the USA shrinks the gum tissue first, and then it falls off again anyways. Is there a way to make the most longer? I have no choice now but to just leave the cap off forever and live with the post.
Hello, Dianne
Thank you for your comment.
Yes, there are a few options for this situation. I am not sure that reducing the gum tissue is the ideal method. The first would be to make a new abutment that is longer, assuming that you have enough room to make a longer post.
Then a new crown can be made that will have enough retention. Sometimes the vertical space is just too small, making this impossible. In that case, the solution would be to make a new crown and post/abutment that is just one piece. These are screwed directly into the implant and they do not require cementing.
If for some reason the implant was not placed far enough into the bone, then the solution may be to lower the gum and prepare the crown margin onto the body of the implant. This is really not ideal but can be a better alternative to removing the implant and starting all over.
I hope that helps to answer your question.
Sincerely,
Dr Balogh
Hello can you advise by any miracle? I had implants done on teeth 11 and 12 a year ago. The xrays show implants to be good, however with the crowns, I have this heavy cement like sensation continuously in my mouth. It feels like a block of rock is sitting in my jaw. They have been removed and remade numerous times and with the crowns it always feels terrible. Thanks
Hello Felicity,
Thank you for your comment.
If everything feels good with the implants and the crowns out, then it probably has something to do with the crowns and their shape.
I understand you have had them remade several times, however, the first thing I would check is the bite. The best way to do this is to place temporary crowns, as they can be adjusted easily.
Then once comfortable the ceramist can duplicate the size and shape of the temporaries. The modifications can then be applied to the final crown.
Regarding your bite, I’m assuming the crowns are adjusted well when you bite on your back teeth (centric) however there may be areas that are still interfering either with your teeth or tongue that makes it feel like a big “block”.
Have your dentist thin the lingual section (back side) even if it does not look to him/her that the crowns are too big in this area. If you feel a difference you will both know he/she is working on the correct area and modifications can be made from there.
I hope this helps to answer your question.
Sincerely,
Dr. Peter Balogh
My implant was losing bone, So my Dr went in with ground bone with my own blood and built it up. but my gum did not heal across the implant. it produced a ulcer between the implant and the permanent tooth. now on the inside of the moth, which I refer to the back of the tooth the skin did not grow from the permanent tooth across the back of the implant to the other permanent tooth. Now on the back of the implant the shaft of the implant is open to the elements. If cold or hot or air touches the shaft it huts a little like brain freeze when you drink something really cold.
My doctor said their will be another procedure. what should I expect?
Hello Yvette,
Thank you for your comment.
It is difficult to say what your dentist plans to do next without seeing the site and knowing
exactly what has been done so far.
The next logical step from what you have described would be to perform some type of soft
tissue graft. If there are no further signs of infection, your dentist can graft new tissue into the area of gum that is not healing.
Sometimes after several procedures or infection, it can take longer for your gums to recover. This is when we perform tissue grafts. In the meantime, try to keep the exposed area clean.
Sorry, I can’t be more helpful. I would need to see the surgery site to explain alternatives.
Sincerely,
Dr. Balogh
I have 3 implants and 1 false tooth where my 4 front teeth were. After 2 years of infections and rejections I finally got my permanent teeth 3 months ago. A couple of days ago I noticed what looks like an irritation on my gum above teeth 7 and 8. Is it possible to get an infection and what will the course of action be? Going to my dentist tomorrow, curious what your thoughts are. Thank you.
Hello Fran,
Thank you for your comment.
This could simply just be some gum irritation, and it may just be from
food collecting in the area. It may not be anything serious but
it should be checked out.
Especially considering your history of infections in the area. If it is the
start of something it is best to fix it as early as possible, so it is good that you are meeting with your dentist.
Sincerely,
Dr Balogh
Hello there,
I have had an implant and a temporary crown placed on my front left tooth the end of August 2017.
The original tooth was root canaled over 10 years ago and was pulled a little over a year ago due to an abscessed tooth infection. I then had a bone graft and an implant placed about 8 months later.
I am a clencher and a grinder. I believe I am pressing on the tooth in my sleep with my tougne and I do wear a night guard on my bottom teeth.
While having my teeth cleaned last week, the hygienist said there was a slight movement in the tempory tooth.
I’m wondering if my bone will still fuse to the implant if there is movement. The surgeon said that it will take up to 6 months to happen but I’m concerned that if there is movement now after 3 months will it still fuse. I also wonder there is anything to protect my front teeth from pressure.
Any information would be appreciated. Thank you.
Hello Christina,
Thank you for your comment.
If your implant is loose three months later the chances of it being
successful are slim. By now if there is still movement, it’s likely there
has been soft tissue that has grown around the implant surface.
However, it could be that the implant is fine but he abutment holding the crown is
loose. In that case, your implant will be OK.
To reduce pressure on the implant the temporary crown has to be adjusted so that when you put your
teeth together and move your lower jaw there is no contact with the
temporary crown.
In order to prevent your tongue from pushing against the
implant at night, you may need a guard for the upper jaw instead.
Alternatively, the other option is not to attach a temporary crown to the
implant and to make a temporary tooth that is either removable or bonded
to the adjacent teeth.
You should get your surgeon to check on the
condition of the implant as there can be several reasons for why it may feel loose.
Sincerely,
Dr. Balogh
Thank you for the information. I have had two implant failures on my number 18. Both times the bone graft and post placement seemed to go just fine. But when the dentist was fitting the prosthetic tooth and tried to to tighten the abutment I experienced a quite a bit of pain. The surgeon wants to try again but I am very reluctant. I am 68 and do not have any health issues that I know of that might compromise the implant. I am now considering having the post removed and just live without the tooth. I still have my wisdom teeth and my teeth are in otherwise good health.
Met with the surgeon. He said the root from #19 runs under #18. He said the problem is the post making contact with my bone and transferring pain to that root. What he wants to do is scrape away enough of my bone to allow for a bone graft to completely surround the new post. Hope that makes sense.
Hello Mike,
Thank you for your comments.
The feeling of discomfort as the abutment was being tightened could be the feeling of the implant turning. If so, then it usually is due to one of two scenarios:
Either the implant needs a little more time to heal and for the bone to integrate with the implant (more likely in cases of poor bone density)
Or there is something that has occurred that has prevented integration from happening over a large part of the implant. It could be soft tissue ingrowth, infection in the area, crowding or a complication within the bone itself.
The other possibility is the implant is perfectly fine, but in tightening the abutment the shape of the abutment is putting pressure on the tissues and bone near the crest of the implant. In the first case, the pain will tend to feel very deep, in the latter it may feel more superficial. In this case, the tissues will often adapt (usually within minutes) or if not the abutment might need to be modified.
Certainly, with only one missing tooth you will still be able to function, we all adapt reasonably well. However, if it truly is the implant it does not mean it can’t be successful. But it would certainly help if the surgeon could identify some potential causes and take steps to minimize them the next time around.
I hope that helped to answer your question.
Sincerely,
Dr. Balogh
Friday morning I received implants on top and bottom. 4 on top and 4 on bottom. The left side of my mouth is not hurting badly but the right side, mostly the bottom is hurting very badly. Like when I had my real teeth and something was wrong with them. I’m wondering if this is normal, they did say I was difficult to numb. I’m sort of living off ibuprofen and Tylenol. It’s Saturday night, this could be normal, yes?
Hello Lana,
Thank you for your comment.
It is not unusual to have some soreness for anywhere from one to three days following an implant surgery.
The extent of discomfort depends on so many factors such as individual pain tolerance, the actual procedure performed, surgical protocol and technique etc.
I expect your surgeon gave you some indication as to what is normal. Although by now I am sure you have recovered, any time you experience something different from what you have been told to expect you should notify your dentist or surgeon. This is just to rule out any other issues and ensure you heal well.
If by chance you are still experiencing this localized pain, there could be a potential infection. That would need to be treated immediately so do not hesitate to notify your dentist.
Sincerely,
Dr. Balogh
Hello Dr. Balogh,
I have recently had some implants put in, and in a week I will be going back for more and to start with final crowns on the existing implants.
I have a dilemma though: My front bottom 4 teeth are missing. Is it best to have 4 implants put in or could I get away with just 2 and skip the implants on the middle 2?
Also, is the estethic result good and will there be any risks of food going under, if I link together one implant with a crown?
Hello Roxana,
Thank you for your comment.
Yes, often in the lower anterior, a bridge is a better option. The amount of space is typically “tight” making it difficult to place individual implants and teeth.
Yes, some food or plaque can get under the bridge (as with all bridges) but this can be mitigated by the design of the teeth. And as long you carefully clean and floss the area it will be fine in the long term.
The aesthetics will be the same and in some cases even better, so no need to worry about that. And it is also more affordable in general.
Sincerely,
Dr. Balogh
I had a dental implant on tooth #9 almost two months ago. I recovered well for the first week, however, began developing tenderness and throbbing pain over the site. Over the next ten days the discomfort became worse. The “flipper” seemed to put pressure on the site and exacerbate the pain as well. On f/u with the oral surgeon he noted mucosal swelling and redness with marked focal tenderness. Antibiotics and chlorhexidine rinse were utilized. Unfortunately, despite complete compliance and excellent oral hygiene, the implant seems doomed! Although the swelling and redness have improved, there is marked tenderness along the anterior mucosal surface and putting on make up, brushing teeth, any pressure, etc will result in pain. Excessive talking, smiling, coughing, etc can result in throbbing. A new device was made in order to alleviate the pressure applied by the initial flipper, which may have slightly pushed the implant cephalad. Even a six day course of steroids was tried. Why will the tenderness and presumed implantitis not resolve? I desperately want to avoid explanting it. What can I do???
Hello Jill:
Sorry to say but it really does sound like your implant has failed to integrate. If an implant is sore to press, touch or loose after even two weeks I would be very suspicious that it has failed. In some cases stabilizing the implant can help if it is caught early, but now that two months have gone by the implant should feel relatively solid and comfortable. There is a possibility that the issue is simply soft tissue inflammation in which case the implant may actually be ok. However, at the same time, you should not even be having soft tissue inflammation at this point in time. IF there is something irritating the gums around the implant it should be investigated and remedied.
Should the implant need to come out don’t lose hope….in some cases another implant can be placed immediately as long as the bone is good, and in other cases, the area may just need to heal a little before replacing the implant? The most important thing would be for a dentist to have some idea(s) as to what caused the initial problem to avoid a repeat occurrence.
Sincerely,
Dr. Balogh
Hi,
I had one dental implant placed 9 days ago. I went back yesterday to get the stitches removed. I’ve been in a lot of pain, still taking painkillers day and night. The pain seems to start in my temple and radiate through my jaw joint then go down around until me front lower teeth. My chin also went numb two days ago and is still numb.
Dentist said there are no signs of infection and some people just take longer to heal, but this pain doesn’t seem right to me.
Any suggestions?
Hello Lisa:
Sorry for the late response. You wrote a few weeks ago, so definitely by now, you should not have any pain or any numbness. Although there may not have been any signs of infection, your symptoms are not so common. I agree that some people do heal slower, some have a higher or lower pain tolerance but overall after 9 days most people would be well on their way to recovery. Without seeing you and knowing exactly what was done it is next to impossible to tell you why you are having this “trouble”.
Not to say that this is what your situation is…. but I had a somewhat similar experience with my very own lower molar. It was fine for 24 hours but then developed moderate to severe pain for two weeks, felt numbness in my teeth and lip and then the symptoms went away after ~2 1/2 weeks. Unfortunately after one month the implant literally fell out. The problem in my case was the implant was placed with too much torque and the dentist could not reverse it. This torque caused excessive strain putting pressure on the adjacent nerve, teeth etc. It caused pressure necrosis of the bone, which eventually reduced the discomfort but then the implant failed as there was “no bone” to secure it.
Hopefully, this is not your situation and without any more details, it is really difficult to say further. Definitely, follow up with your dentist especially if you are still having symptoms.
Sincerely,
Dr. Balogh
Hi,
I had one dental implant placed 9 days ago. I went back yesterday to get the stitches removed. I’ve been in a lot of pain, still taking painkillers day and night. The pain seems to start in my temple and radiate through my jaw joint then go down around until me front lower teeth. My chin also went numb two days ago and is still numb.
Dentist said there are no signs of infection and some people just take longer to heal, but this pain doesn’t seem right to me.
Any suggestions?
I had an implant last June 2017, it passed the “stress test” in January 2018 and the surgen gave me the ok to have the regular dentist add the tooth to the post. The regular dentist fitted the tooth and said everything looked fine. At the same time he removed a deep old filling in tooth #14 which is right infront of the implant and ground it down, filled it and placed a temporary crown on it. The two teeth will receive the crown the same day. There was “normal” pain from having a tooth filled, but it was painful to bite down on the #14 tooth and it lasted for more than a week. That is slowly subsiding, but for the past 6 nights I have been awakend by pain going across my face under the cheek bone. The surgen is out of the country for three weeks. I called the regular dentist but he was a bit dismissive and told me to check with an endodtotist for possible root canal of tooth. I find it hard to believe it is a root canal causing pain across my face along the legnth of the check bone. Any advise?
Hello Rich:
Most likely your dentist is correct…the #14 probably does need a root canal. It is not unusual for a tooth to cause referred pain to the opposite jaw, top of the head, ear etc. It would be very unusual for this pain to be coming from your implant.
Sincerely,
Dr. Balogh
I had 2 implants the same day in July 2017. One of the implants was done immediately that tooth was extracted which was my left wisdom tooth. Since that time, I have been having tightness on left side of my 4 frontal teeth and also on the gum below that teeth, skin on that jaw is affected too. I feel numb on my jaw and sometimes pain on the gum. The teeth is very sensitive when brushing. When I eat cold food, the coldness will penetrate from inside to outside of the affected side. Left side of my lip is affected. When I touch that side, I feel very cold and sensitive. Please I need your help. Thanks.
Hello Frances,
It is really difficult to guide you as I have a lot more questions than answers. Without knowing exactly which sites were implanted…upper or lower wisdom teeth, and where was the second one…and exactly which teeth are affected, where the numbness extends, when the symptoms developed etc it is difficult to discern very much without risking giving you completely erroneous and incorrect advice. Some of your symptoms such as teeth sensitivity could be “normal” and unrelated to your implants; the best solution would be to return to your dentist and explain your symptoms and if he/she cannot identify and determine the cause and solution to your issues ask for a referral.
Sincerely,
Dr. Balogh
Hello. I had all my lower teeth pulled in preperation for a full denture with implants. My dentist was able to insert 3 implants to hold the denture. We are now 6 months later and inserting the final implants and fitting the denture. When the denture is “snapped” in it is VERY painful on 2 of the implants. Also, when one side of the denture is snapped in, the other side gets raised up and will not snap in. I now have had to stop using the plate and unscrw the anchors.
Can you shed any light on my situation?
Hello Kristy,
The first item to discern is whether the pain is coming from the implants themselves or the tissues. Most likely it is the tissues because if it was an implant then even just pressing on it with your finger, an instrument etc would cause pain…and that is not so likely after six months of healing. So the denture is probably pinching or pressing too much on the gum tissue as it is inserted. The reason why one side flips up is either because the implants and the attachments are not parallel enough and hence not engaging the clips fully, or the clips on the denture side were not attached in a fully seated and passive position. The latter issue is easy to fix by reattaching the clip on the denture side. The former may require using an angled or customized attachment to make the clips more parallel.
Sincerely,
Dr. Balogh
I had all my lower removed about 2 weeks ago. They then placed 2 implant in and gave me my temporary teeth until it heals. I have little to no pain but I do feel a lot of pressure from the very front of my mouth. Is this normal?? I also feel one implant is higher than the other which is making my teeth not fit. I follow up soon with my doctor but until then I won’t know anything
Hello Jenny:
You shouldn’t be feeling a lot of pressure from the implants per se. However the pressure could be from the feature pressing on the gums as they heal.If that is where you perceive the pressure it is normal and should go away soon. If it feels more “internal” it could be pressure being placed on the bone from the implants. That should also go away within days…however if there truly is excessive pressure I am sorry to say it may lead to something called “pressure necrosis” in which case the implant may fail to integrate.
Dr Balogh
Hi Dr. I have received a bridge that connects to impants I was told they just snap out to clean but why can’t I do this they don’t come out what should I do to get them out? Thank you Nancy
Hello Nancy
Some prosthetics are designed to be removed but he patient and some are meant to be”permanent’ or alt least not removable by the patient. Usually bridges are designed to be non removable, but best to confirm with your dentist. There’re pros and cons with both types and which one is best varies with the specific needs and desires each patient, as well as what is best for long term success
Sincerely
Dr Balogh
I had an implant done on tooth #19 approximately10 years ago. A few years in, it developed a pocket, the periodontist opened a flap and cleaned it out. A few years after that, it developed again. The implant was removed. After much thought and a consult with another oral surgeon, I decided to have another implant placed. The second implant was done approximately two years ago, the crown was place approximately a year ago. Now it has developed another pocket. My oral hygiene is good, and I use a water pick every day. I have another implant on the opposite tooth #30, which was the first one I had, and have never had a problem. #19 feels fine and I haven’t had any problems. There was a bone graft done prior to both implants. There is only one thing different, I have mentioned this to the dentist, but it seems unimportant to him. When I use the water pick on this tooth, and only sometimes not all the time, the gum around the tooth feels “loose”. Sometimes it just seems as though I can feel the water go below the gum line. Otherwise, there is no pain, nothing else to indicate a problem. I have been instructed to irrigate with Perioguard and to return to have it checked in 3 weeks. If you could shed any light on this situation, what is causing it, and what could be done to “fix” it, I would be grateful.
Hello Linda
Without seeing the area in particular I can only guess….however here goes. Long term bone loss around and implant currently is attributed to a few most common issues…too much force on a given implant and food impaction and the inablility to clean./ I cannot comment on the former, and the second it sounds like you are doing everything you can. However your description of the gums is “interesting”. Once again I cannot say for sure without seeing the clinical situation, but it may be that there is alack of attached tissue around the implant, some muscle pull, a very deep pocket or a combination of the above. This would allow bacteria to ingress into the area around the implants when you eat and drink etc. If that is the case then some gum grafting or gum surgery may help to rectify the problem. As a more conservative approach, continue to waterpik but use somethign tjhat is antibacterial in the waterpic…hot salt water or baking soda water is a good start
Sincerely,
Dr Balogh
Hello ,
I am 69 , very lean and have four unhealthy looking teeth on my bottom front of my mouth . I wear a top plate .Hx of smoking, throat cancer and bowel ca over 10 years ago . I smoke medicinal marijuana frequently and drink fairly heavy, most days of the week . I quit on occasion. I can eat steak, apples to carrots as my gums are low and tough . I had implants about five years ago in Mexico which all fell out . ( my late wife’s implants were a success ) I am considering getting dental implants in Thailand . I’ve heard they are known for good prices and have good success. Will I require a long stay ?
Regards,
Dennis
Hello Dennis:
As a general rule I want to see patients for a post operative visit after 10-14 days. In most cases if at their initial post op visit everything has been routine and normal thenI won’t need see them again for at least 3-4 months. However, with your past history I would be more concerned about your initial healing…so if it was myself I would want to be able to follow up with you for the first month. However another dentist/surgeon may feel differently and once they have a chance to exam the site, your bite, gums etc that could change also. Hopefully this helps a little. You may want to reach out to the dentist you are planning to see. They may be able to give you more accurate information once they see. your detailed history, x rays etc.
Sincerely
Dr Balogh
Dear Dr. Balogh,
Thank you for this very informative website. July 2017 I had an implant installed to replace tooth #13, which had been extracted over 10 years ago. I recall at the time there was some concern by the periodontist whether I had enough bone structure to hold the implant, but all went well. I’ve had no issues or big problems- just a slight discomfort when putting pressure on the tooth, or drinking cold liquids. Jan. 2018 I went for regular exam/cleaning and after mentioning the discomfort, the dentist filed the implant down a little, which seemed to help. However, the real tooth directly next to the implant has significant gum recession and he scheduled me to consult with the oral surgeon to discuss options. That was yesterday and what a mess! The oral surgeon took one look at the X-ray, never even peeked inside my mouth and declared I needed to see the periodontist who performed the implant, ASAP! (Then promptly went to lunch without explaining anything to me.) I now have an appointment with the original periodontist next week, but in the meantime, am worried something is really wrong and scared to death of a potential bone graft. Still NO looseness of that tooth and just kind of a dull ache on the upper side of my face. (Sorry this post is so long!) What do YOU think?
Hello Pam
It is really difficult to say what the oral surgeon saw….I’m guessing saw some bone loss around the implant. However until you have it seen it is really difficult to say whether or not it is something simple or challenging to fix. In the world of implants there is a huge range of experience, training and understanding more so than other fields of dentistry…so what may seem like a big problem to onep erson may be easily remedied by another.
Sincerely,
Dr Balogh
I had an implant done in #26 and it failed. There was an infection and severe bone loss in the area (the gum dips down between #25 and #27) I had that implant removed then had a horizontal bone graft done, But the vertical bone loss was still there.I had a second bone graft done and a second implant (a narrow one) placed in that area. However the vertical bone loss there is still visible. Almost a year later, I haven’t had a crown placed but the second implant that was done seems more exposed and I noticed there is some micromobility of the implant (forwards and backwards). Does this mean the implant has failed?
Hello Brian:
Sorry to say but if there is movement of an implant even after 3 months it most likely has failed. In some rare situations it may be able to “save” the implant but usually it is best to remove it,cleanthe site and replace it with anew one.
Sincerely
Dr Balogh
I have implants in top row front teeth (since 2006). Is it possible to have implants placed for permanent dentures for my remaining upper plate? I’ve seen 2 different dentists one says and there says no. Going to third dentist for deciding action, I hope.
Hello Chris:
I’m guessig there could be two challenges…one is that you lack bone in the posterior. The one dentist might not know how to overcome the problem so felt that the implants would not work. The other issue is the location and angulation of your existing anterior implants might make fabricating adventure over top difficult or challenging. Hard to say more without knowing more information
Sincerely
DR Balogh
Hello
I have an implant on my front tooth and all has been fine for 4 years, until I got pregnant. Now in my third trimester it bleeds a lot , the gum , mainly at night , my dentist today advised me to go back , I have a very strict cleaning routine and my dentist thinks there is a gap between the crown and the implant perhaps? That allows food to get in easily , so it doesn’t matter how vigorously I clean it bacteria still gets in. I have made an appointment to go back to my Implantologist but I’m feeling very distressed and wondered what the worst case scenario was? Will I lose the implant?. I had an x Ray in April last year (just before I got pregnant ) and the bone looked good .
Thank you
Jerry
Hello Jerry
It does not sound like you will lose the implant. It is well known that during pregnancy the change in hormones causes more bleeding and inflammation of the gums.On the other hand if there is an area of food impaction it can lead to bone loss despite pregnacy, so you should get it check and fixed if possible.
Sincerely
Dr balogh
I was in 10 out of 10 level pain for w months after having all of my teeth removed and getting full upper and lower sets of implants. They were in a bind when they were placed and set. The dentist used permanent glue to attach the teeth to the posts. Now, six years later and after losing 6 posts due to bone loss and infection I am in terrible pain and found out via x-rays that all of the remaining implanted posts have bone loss and infection. Due to the permanent glue the dentist has to cut the posts out through my gums and saw the post off where it is glued to the porcelain teeth. Isn’t there a better solution to getting these out of my bone and what happens next? What should I do?
Hello John: It sounds as if something was amiss when your had your first surgery with the extractions and implants…you should not have had sever pain for months afterwards. As far as why your implants are failing after only six years, there are lots of possibilities but without having more information it is impossible to say. Failing implants can sometimes be saved if the bone loss is not too great. And to be able to salvage or remove an implant we typically need to be able to remove the teeth above it, and if they are cemented they often will need to be cut off if the cement used was a very strong one. Regarding what to do next…firstly is to make sure your dentist has a clear understanding why you had so many problems in the first place, and then make sure he/she has a different solution to avoid a repeat occurrence. You may need some bone grafting if there is not enough bone and/or you may need to consider a different type of prosthetics for the final teeth. Sorry I can’t help more but I just don’t have enough information to guide you further.
Sincerely, Dr Balogh
Is there a way to remove the teeth sections from the posts if permanent glue was used?
Hello John: Sometimes the cement seal can be “broken” by using ultrasonics to vibrate the posts and other times tapping can loosen cemented abutments, but without seeing your teeth and implants it is difficult to know.
Sincerely, Dr Balogh
Hello I had four implants placed in the top of my mouth while my teeth were pulled out I have no problem with the implants but it was called for on one they do not stay and they keep on coming loose why would that happen is the enbutment Worn out and Dentist keeps on saying there’s nothing wrong every time I eat they move if I chew on the left the right comes up if I chew in the front the back comes off I paid $22,000 for this is this wrong should they stay in tight there’s supposed to be able to be pulled out but they’re supposed to stay in tight that’s the reason I did it please tell me if my dentist is doing the wrong thing
Hello John
There are many possibilities…the type and tightness of the attachments are one aspect that may need to be changed, the set up and bite of your new teeth is another, and thirdly the fit of the teeth against the gums is another possibility. Your dentist should look at all these things and be able to determine which of these are contributing to your tooth movement.
Sincerely,
Dr Balogh
Deae Dr. Balogh,
I had my initial implant surgery done in October. Yesterday, I had the abutment portion of the procedure
Performed. Despite almost no pain or discomfort from the initial procedure, I
Am now in a considerable amount of
Discomfort. The gums are really achey. I asked my dentist before leaving the office if there were any care instructions or foods to avoid but he said no. He is usually a very thorough dentist so this confused me.
Do you have any advice? I have taken tylenol but it has not helped.
Thank you!
Hello Rebecca: Not sure why your gums are so sore without knowing exactly what was done to place your abutment. Take some ibuprofen as an pain killer and anti-inflammatory, but if it persists beyond one to two days notify your dentist.
Sincerely, Dr Balogh
Hello,
I recently got implants on two front teeth and have had some gum issues on one implant. I went to my periodontist, had X-rays done and they were fine. He recommended using a different toothbrush to really clean the gums and a mouth rinse twice a day. It has since cleared up the redness and pain however now it seems that I have a tiny black spot on the top of the gum, it almost looks as though the abutment is starting to come thru. Can this happen due to brushing? If so, will that heal over? I did not have any issues with my gums healing during the implant process.
Thank you.
Amanda H.
Hello Amanda: Without seeing the area it is difficult to say…but I am guessing that you had some inflammation (redness and pain) and now that that has subsided the gums have healed and “tightened up”. In doing so they often shrink a bit and you may be seeing the edge of the crown or abutment showing through. Really heavy brushing could also cause some recession but more likely over a longer time period. Unfortunately if I am correct about the gum recession it probably wont reverse without some type of intervention. Sincerely, Dr Balogh
Hello. I had an implant placed in my lower left jaw on Feb. 3 (it is now Feb. 15). I have not yet regained feeling in my chin and lower lip. My lip feels tight and cold while my jaw feels quite full.
I do not have as much swelling as I did the first week, but it feels like it is huge. My tastebuds seem to be affected, although it could be my imagination. I am a college professor and I talk all day; sometimes my jaw becomes sore, other times I struggle to say words correctly because of the numbness. The dentist said that it takes a while to get feeling back – up to a year. What? I had a 5-day check up and he said everything was fine but he didn’t even look in my mouth. I feel like I’m rambling but I’m really stressed out about this situation. Any information would be greatly appreciated.
Regards,
Kerry Ford
Hello Kerry: Your dentist is correct that nerves do take a long time to heal, in some cases up to one year. Fortunately we don’t see nerve impairment often but when we do we try to assess what may have occurred and why. If there may have been some trauma during surgery then a short duration of corticosteroids can help reduce any inflammation. If it is thought that an implant is impinging or causing too much pressure then it may be best to remove it, allow everything to heal and then carry on. Sometimes there can be temporary numbness due to initial inflammation, but then after a few days or ~2 weeks of healing sensation begins to return and often is back to normal within 2-3 months or less. If there is still total numbness after 2+ weeks and you don’t have a follow up appointment arranged, call your dentist. You may need to get a ct scan to determine the exact position of the implant to the nerve to rule out any impingement. Sincerely, Dr Balogh
Seven months ago I had an infection in a molar, I took antibiotics and right after the molar was removed and a bone graft performed using cow bone. The graft was unsuccessful. The bone was lost 3 mm. to the sinus cavity. The site of the molar was very swollen and maybe infected, it took about 6 or 7 weeks to heal.
I am looking into do implants. The four upper molars of the left and right. The dentist wants to do them all at the same time. I am afraid that if I had problems healing from one extraction, what can happen when my body tries to heal four implants at the same time. Isn’t this a bit too dramatic? Should I do just two teeth at one time?
Please help, I am very stressed out.
Hello Maria: It is not unusual or “too much” to place four implants at once. In some cases I have placed 14-16 implants in one appointment, and in some cases that also included grafting and extractions. In my experience we see more complications following some extractions than implant surgery…and in your case your dentists was dealing with a preexsiting infection.Speak to your dentist about your concerns, however there is also no harm in doing one side at a time other than you have to have two surgeries. Sincerely,Dr Balogh
Hello Dr. Peter Balogh. It is so nice of you to give such valuable recommendations. I wish I would live closer to your practice.
I just had one implant placed two weeks ago. It is one of the molars in the back of the upper jar. The third one from the back. My original tooth was in a very bad shape, fractured root which caused bad infection involving even gums around. Before the implant, I was placed on amoxicillin for 7 days but did not responded much. CT scan was done and my dentist told me that it was close to sinus, but he was planning to put some material or bone graft ( i don’t remember the name of it) to help my bone to grow. After performing surgery, and cleaning the area very well, he placed an implant and gave me to take for 7-day amoxicillin again. After leaving his office I noticed that I have sinus drainage which was clear. I got an instruction not to blow my nose, that I thought I followed. I did not have much pain during healing and I felt that I did well. However, two weeks later after I stopped antibiotics I noticed that I have yellowish secretions coming from my mouth. I feel that I have a post nasal drip that comes from the same area where is my implant. Every day the drainage increased. Today I went to my dentist, the implant doctor was not there. My dentist took pictures and told me that she will talk to the implant doctor. She noticed that my gums around that area (on the inside) are inflamed and gave me to take Clindamycin for 7 days as I’m allergic to Augmentin. Now is my question, I’m concerned that the implant went through my sinus an infection is developing there now. What do you think, and what needs to be done in your opinion?
Hello Yovita: Definitely follow up with your dentist and the one that did the surgery within the next week, especially if your symptoms do not go away. Without knowing the bone volume, density in the surgical site and how secure the implant was at the time of surgery, and where the implant “is”, it is difficult to comment on what has occurred. It is very rare, although not impossible for an implant to become displaced after surgery. Sorry this may not have been as helpful as you had hoped. Sincerely, Dr Balogh
Hi, Dr Balogh
my anterior incisors (two middle lower ones) have gum loss. This is due to having braces at a late age (late forties). this happened 15 years ago. One is very loose, This one shows the most gum loss. the other one has little gum loss. I want to have the loose one replaced with a implant. I know this is a tight area. Can it be done? My dentist wants to do both of them.
Also, what is your opinion on gingival graft? Thank you.
Hello William: A gingival graft can be good thing if it is being done for the right reasons. However if your tooth is very loose, it is probably due to lack of bone or something affecting your bite or even a combination thereof. A single implant can often be placed but it is a tight area. Whether you place one or two implants will depend on the condition and prognosis of both teeth and the feasibility of placing implants. Often because the space is tight I will place a single implant and then place two crowns on the one implant (cantilever bridge). We would not normally do this in a functional area such as a molar but it can be done in the lower anterior with good success. Sincerely, Dr Balogh
Hi Dr. Balogh,
I have a front partial dental bridge since 10 yrs. ago. On Oct. 2016 The corner of a flat sheet of plastic accidentally got under and the gum, in between the gum and the tooth with the bridge. Since then I had complications on the gum. I went to the dentist that did the bridge a few weeks right after. He did a cleaning and gave me antibiotics but the inflammflamed gum didn’t go away. I went to another dentist did a cleaning too but had no success whatsoever to heal the gums. They thought it was a gigivital imflammation. I went to another one and again was sent home with peridex mouth wash. I finally went to a periodontist. She did surgery to clear the infection, send me to an endontist to check the root canal but didn’t find an issue with it. She said I was showing some bone loss at the beginning I went with her, did the surgery and scraped excess cement. The gums started to heal for a little bit back in March 2017. But then I felt that I reinjured it and it went back to gum imflamation and the two real teeth next to the bridge were surgery was done are sensitive since the surgery. I went back in January and x-rays show I have bone loss and she said it the whole bridge needs to come off and the two teeth attached to it. Now I have pain on the side of the nose and goes up to the bottom of the eye. It feels like an itching sensation on the side of the nose. The sensitivity on the real teeth is on going. Mean while the periodontal Dr. a cosmetic dental Dr. And a orthodontist are teaming up to discuss my case. They’ve proposed a procedure where I’ll have the bridge and the teeth attached to it removed, let gums heal then go for dental implants. But since I have a 9 ml. overbite I consulted the orthodontist to correct the over bite then get the implants done (if it’s possible). With your experience of practice, what would you do with my case? I need a second opinion, I’m so overwhelmed and heart broken at the same time. It’s been trying to heal from more than a year now, I don’t want to keep on loosing or extracting teeth I just want my dental health back. Since the bridge was done I felt that my overbite got wider, i have calluses next to the moles, on the gums. I been chewing on that’s side since the bridge was put on. I have an accent too. I have no symmetrical mouth do to the wider gap on the side wehere the sensitive real teeth remain. Now, my gums on the bridge are aggravated and the pain on the one side of the nose. I’d like to address all this issues? Do I have more than one option? Thank you.
Hello Lineth: Your case sounds very complex and I would think that with the many specialists that you have working together they should have you on the correct path to health. This is only a guess, but if you had a 9mm overbite the lower teeth may be impinging on the gums of the upper teeth, and if so this may have been a big contributor to your dental problem. I don’t know how old you are, what the rest of your bite looks like and what your aesthetic situation is etc…so a lot more unknowns and questions to really give you good advice.However, based on what I understand definitely look into orthodontics to see if that will help your bite, esthetics etc….if soit should be done first v=before any implants
Sincerely, Dr Balogh
I had the crown placed for my implant yesterday. It is shorter than the adjacent teeth which seems odd. Also, there is pressure on the teeth next to the crown causing those teeth to shift. As a result I am unable to get floss between several teeth. Are these issues common? I called the dental office and I was told the other teeth will become more in line with the implant because I have not been eating on that side. Again, that seems odd and I have been eating some on that side. I would love some input regarding these questions. The tooth is in my upper right side third tooth from the back.
Hello Therese:You should find the pressure will be received within a day. However, if you still feel pressure or if you cannot floss without tearing the floss beyond 1-3 days then the contact may have to be adjusted. It is relatively easy to do. There are some reasons why an implant crown is slightly lighter contact than natural teeth, but usually it is so small it is not visible.See how you do safari as chewing on that side…if you find that you are not getting enough contact or chewing function let your dentist know and they can probably build up the surface.
Sincerely, Dr Balogh
Hello Therese:It is not unusual to feel some tightness or pressure between the teeth for the first one to two days. However if it continues, if you feel discomfort on your adjacent teeth or you find floss shredding then the crown probably needs to be adjusted. The adjustment to the bite is important but it usually does not have to be visually shorter…ask your dentist about why it was done that way and if it can be modified
Sincerely,
Dr Balogh
I had implants done in October 2017 . All healed well . I went last week (February 2018 ) to have the crowns fitted . The dentist really screwed them in tight . The following day I started to have throbbing on what felt like my lower teeth below the implants . No binding or pressure so I thought it was a filling which had cracked . Went back to the dentist in pain and she replaced the filling and told me it had been leaking . Still in a lot of pain which radiates from my ear and throat to my jaw . Sometimes it feels like the implants are sore and sometimes I think it might be an abscess under the lower back teeth . Eve,n now it feels like I have a severe case of ear ache . I am taking pain killers but I cannot keep,on popping tablets and powders . Might it be an ear infection ? Wish I could find out exactly what is causing my discomfort as the dentists cannot find the problem . They tap and blow cold air and give me cold water to drink and nothing . But the throbbing persists .. Any suggestions ?
Hello Michael: You should have your bite checked. It can seem like the bite is correct, however there may be areas where your teeth make heavy contact that are not obvious at first. You may clench or grind at night and this could add to the problem. Teeth will compress ~30 microns upon clenching, whereas and implant will compress only 3-5 microns depending on bone density. So an implant crown which appears to be OK under a normal bite will be high upon clenching….imagine having a pebble in your shoe…that part of upper foot will become sore almost immediately. Also have your dentist ensure that “there are no contact points in what we call excursions….there should be centric contact only and it should be light to shim stock.”
Sincerely, Dr Balogh
Hello Michael: One of the most common issues is having a heavy bite…sometimes even when a tooth appears to be “normal” using the carbon papers and other items to check the bite, I ahve found that a bite adjustment has solved the problem, basically teaching me that even when things look perfect the bite an still be too high. Another possibility is that there is something wrong with the lower tooth and it simply did not have symptoms until it was put back into function. I really do not feel that this is related to your ear/infection. If it is still sore, have your dentist reduce the bite, or alternatively remove the crown for a few days to see if there is a correlation
Sincerely
Dr Balogh
Hi,
I had two implants done (April 2016) on my teeth no.9 and 8 and everything seemed OK. around August that year I started having pain on implant no. 8 and even lifting my lip or talking was painful , I saw several oral surgeon and all said everything seems OK and there is no bone loss and infection there. One oral surgeon agreed to cut that area to put some bone graft there (March 2017) and see if that helps. surgery went well and no complication. After bone graft placement the pain got 20% better but this throbbing effect was added. If I lift my lip or if I rinse my mouth it`s like electricity is running there and it lasts for 10-20 seconds and then it comes down. I also have seen pain specialist and was recommended Lyrican but none helped. I know I shouldn’t have the second surgery(bone graft) and it is just manipulated that area and made everything worse. What is your opinion on that?
—
I also had an epico done on my tooth no.10 and again everything seemed OK and infection is gone but the pain and discomfort got worse than before the surgery. Before the surgery I only had burning sensation now it is pain and discomfort especially when I talk or eat. The pain settles down sometimes but as soon as there is a slight hit to the teeth the pain starts. What do you think cause the problem?
I have grinding problem and use custom maid nightguard at night.
All theses problems started after I had a hit to the face and my front teeth.
Hello Sayeh:Your symptoms are not common…I would agree that the symptoms do not seem to be consistent with infection or even lack of bone. I am curious what the one surgeon found or diagnosed that made him/her feel you would benefit from a further bone graft. I’m guessing that this has already been done, but essentially the entire area needs to be mapped to determine if there are any trigger sites or locations that initiate the pain; a ct scan to evaluate the implants, bone and adjacent teeth; cold or ept tests to determine if there is viability of adjacent teeth; a thorough evaluation of your bite. Sorry this is not very helpful but in this case without seeing the situation in person it is very difficult to give further direction.
Sincerely,
Dr Balogh
Hello Dr. I just had 2 crowns cemented today after the implant healing process. (Upper front teeth). One, they seem slightly shorter than my real teeth and there are gaps between them. Will my gums grow or adjust around them?My dentist tried to convince me they looked perfect. Can they be adjusted to look like my teeth after being cemented?
Hello Victoria:
Without seeing the teeth myself, I cannot say one way or the other regarding the gaps…it is possible that in some circumstances the gums will fill the area in and if so it will happen within a 1-2 weeks (if not sooner) but typically only if it is very small amount…regarding the length you we sometimes have to make the teeth lighter on the biting surfaces but for esthetic reasons we usually do not wish to make the teeth shorter..best to ask your dentist aobout the length.
Sincerely
Dr Balogh
I’ve just had dental implants and a bridge and the gum is really sore under the front teeth what can I put on it to ease the pain
Hello Gill: If the gums are sore it could be initial soreness and inflammation from the surgery; alternatively it could be the bridge is putting too miuch pressure on the tissues…either way the discomfort should reduce fairly quickly after 1- 3 days…if not then call your dentist to let them know. In the mean time, you may wish to try Ibuprofen and salt water rinses to ease the discomfort
Sincerely
Dr Balogh
Would like your opinion here. 🙂
#30 and #31 are both implants. (approximately 20 years for #30 and 12 years for #31) #31 is Straumann, #30 Branemark. Pano taken yesterday with no bone loss present or other radiolucencies. Crowns are splinted together because of the interesting placement of #30. I’m not sure why there is pain when chewing on #31. If the implant is broken, would this cause pain? Also, lower right lip and tongue are numb. Not sure what is happening with these implants. Any suggestions? Ibuprofen and Tylenol help the pain.
Hello Samantha: Sorry for the very late reply. The numbness is suggestive of inflammation or something affecting the nerves…the unusual thing is these areas are affected by two different nerves with different pathways. The lack of bone loss is excellent…however you could have pain if there is a fracture as the pain would be coming from inflammation in the tissues and/or bone. has your bite been checked….I reccently had a patient who was advised to have her implants removed…a simple bite adjustment fixed the problem within 2 days…the other dentists checked her bite also but did not recognize the source of the interference/problem.Have they checked your muscles of mastication? Could be sign of grinding/clenching/bite issues. Nightguard? One option would be to remove the crowns temporarily and see if your symptoms change…may help with diagnosis
Hello,
I have been missing my front tooth (#10) for more than 10 years ever since I was a little kid. I am now 21 years old and considering a dental implant. There is significant bone loss in the area where the tooth is missing. When i went to a dentist referred by my orthodontist, the doctor told me that I have to have bone grafting done before he can place an implant and that i have a 70 percent chance of successful result since I am young and have no other medical issues. He mentioned that even with the bone graft, there might not be enough bone remaining after healing. Not satisfied to hear such low chance of success rate, I went to another dentist for a second opinion and he said that I do not need bone grafting and that he can place an implant at an angle right now so that he can place the implant where there is enough bone. However I wasn’t sure if this procedure is common and safe long-term and started doing some research. I was wondering if what the second doctor told me is relatively safe in the long-run. Currently I am not so sure which way is the best for me. Any advise or explanation will be greatly appreciated! Thank you!!
Hello Jay: Sorry for the late reply. Both docs may be correct….however there is an ideal position for an implant both from an esthetic and functional and health point of view. sometimes we can tweek the position of an implant slightly by changing the angle or moving it slightly. However too much may compromise the look or longevity….without seeing the area myself it is difficult to say who is “most correct”. Overall without having more information I would lean towards the grafting, but best to aks both docs the exact same questions and see how they respond
Sincerely
Dr Balogh
Can a bad/dead tooth kill an implant that is next to it? My mom had 2 implants on her left bottom teeth for a bridge, 6 weeks after surgery she complaint that the front tooth next to the implant hurt and had gone to see her dentist and oral surgeon, she was given antibiotic and oral rinse. 2 weeks after, the implant next to the tooth started oozing and she was told that the bad tooth had killed the implant and the implant was removed immediately. Now, the other implant toward the back is not looking too good either, can the bad front tooth effect both implants even the one far in the back?
Hello Linh:
Yes…if there is an existing infection in a tooth or the bone next to an implant, the bacteria can travel to the adjacent site adn cse the implant to fail. therefore if we see or suspect an infection in a tooth adjacent to a future implant site, the problem should be fixed before any surgery.
Sincerely
Dr Balogh
Hi Doc Balogh,
Good day!
I had my dental implant on the front last April 2017 and it went perfectly fine. However, just recently, I noticed that it’s becoming loose and it slightly moves whenever I close my mouth (my upper and lower teeth meet). I am planning to pay a visit to the dentist but I would like to understand why it so happened even I didn’t put pressure on the teeth when biting this whole time. Thanks.
Definitely see your dentist asap….not sure why it would be loose, but it truly is the implant something has prevented it from integrating with the bone. It does happen sometimes even if we do not chew on it…too many possibilities and too many unkowns for mer to comment further.
Sincerely
Dr Balogh
Hello,
I have a permanent tooth inside my lower jaw. It did not come up. I had my milk tooth extracted. Now that space has to be filled in. What could the possible complications be, if I opt for implant over bridge? (Remember I have a tooth inside my gums).
The tooth may have to be removed and the site may need some grafting if the tooth is in the same position/location as the proposed implant.
Sincerely
Dr Balogh
after 5 years of implant, one crown disconnected, what procedures are necessary to reattached, curious if it means removing implants and or will it be painful?
Hello Pauline
The implants are probably still OK…you may just have to hav ethe teeth removed adn either remade or repaired. If that is the case it should not involve any surgery and should not be uncomfortable/painful.
Sincerely
Dr Balogh
Hi. I need 2 implants on my upper left 7 8 6. All 3 teeth ate extracted. But I can afford only 1. If i go for only one will I still have bone loss issue and will my other teeth fall out bcoz of so many missing teeth.
Hi Sam: You will get bone loss in the area where the other teeth are missing. Another consideration isto have both implants placed now but delay the final teeth. At least the implant (even if not restored) will preserve the bone.
Sincerely
Dr Balogh
Dental implants are a positive addition to oral health.We face many complication during dental implants Risks include: Infection at the implant site. Injury or damage to surrounding structures, such as other teeth or blood vessels. Nerve damage, which can cause pain.
Hi, I had #14 extracted in November. I need to go in for a minor sinus lift and implant but have to wait about 4 more months to save enough money. Will I have less likely of a success rate waiting exactly a year after extraction? What are the odds of sinus irritation and complications after a sinus lift?
HELLO Cher: You may lose a bit more bone due to atrophy by waiting a full year, however I have found that the manta varies considerably form person to person. Some of the reasons for the differences may be the persons own metabolic, although local differences are also a factor. the best thing would be to ask your dentist….I have had some patient ask me the exact same type of question…in some cases I can tell them that delaying will not change the amount of grafting, prognosis or outcome…in other cases delaying beyond a certain length of time is not recommended.
Sincerely
Dr Balogh
I had two lower back implants placed yesterday. I cannot get floss in between them or the tooth next to the second one set. I feel pressure from those to the middle of the bottom front teeth. Is this normal and will this lessen up?
Hell Sharon sometimes the contact between the implant and a natural tooth can be a bit tight at first, however it should loosen up and be flossable within 2- 3 days at the very most. If not, go back to your dentist…it is an easy problem to fix…the corns just need a slight adjustment and polish.
Sincerely
Dr Balogh
I’m in the process of getting dental implants for my 2 upper front teeth. I just had my first implant crown placed in. So now I have one tooth and one missing tooth next to it. The implant crown keeps rubbing against my upper inner lip. Went back to the dentist and he told me it’s because i’m missing the tooth next to it. He said that when i get the other crown placed next to it, i should be fine and that I will not feel any rubbing on the upper inner lip. Is this true? I have no pain but its extremely annoying. Thanks!
Hello Themistoklis:
It could be that the one missing tooth causes your lip to “fall in” and therefore catch or rub against the crown. ON the other hand, it could also be the size, shape and length of the existing crown…one way to find out is either to wait until the other crown is inserted or make a temp crown, temporarily bond it into place and then see if the problem is resolved
sincerely,
dr Balogh
I have multiple any plants that have been placed during the last 20 to 30 years. I continue to have a lot of Need for dental service and I’m considering implants for dentures. Would it be possible to use the current posts or would they have to be replaced to have them be used for dentures?
Hello Caren: you should be able to use the existing implants, although the posts/abutments that now hold the crowns will likely need to be replaced. Sincerely, Dr Balogh
I got eight dental implants, 2 in each of the back four corners of my mouth, in July 2016. The year prior I had a double sinus lift, 4 extractions, and a lot of bone grafting due to congenitally missing teeth. One year after the crowns were placed I started having issues around the bottom back right implant. The gums on two side have a sensitive/painful sensation that is worsened by pressure or even a light touch. It pretty much bothers me all the time. My oral surgeon, dentist, and a periodontist have all brushed me off saying there is no bone loss and the gums look “textbook healthy”. I think the pain is from the bone grafting causing little boney bumps under the gums. I can’t get anyone to help me and they want me to accept that it is an anomaly or nerve pain. When I had the screws placed I had to have 4-5 sharp boney nodules removed from the top gum area, but it was not painful or sensitive like the bottom area is. I don’t know what to do and any advice would be great. I feel like it has to be something somewhat correctable because the other 7 implants are fine. Help!?!?!
Hello Stephanie:
Because the issues started one year after the crowns were placed the first thing that should be checked is your bite. Although the bite may “look” OK visually, sometimes the lower jaw flexes as we chew, bite or worse if we clench. Your bite should be checked while clenching and while grinding side to side. The bite should be adjusted so that it is slightly out of occlusion and see if that makes a difference. The other possibility is that there is some bone loss developing around the implant or a lack of integration/bony union of the implant and bone. If that is the case then unfortunately it will come more clear as time goes on and you may lose the implant.
You do bring up an important point…why to of 8 implants does only one hurt. I can say that pain is not normal with implants…there is something going on, although it is not always easy to identify, especially at the beginning stages.
Sincerely,Dr Balogh
Dr. Balogh. I had a root canal fail after about 5 years. It was redone and failed again as it was determined that the tooth root fractured. April of 2018 I had the tooth pulled. I had a dental implant placed in my lower right jaw (pre-molar) in July 2018. It is 10/26. About 2 weeks ago my dentist placed my crown on the abutment. When they took the healing seal out I could feel it in my tooth. When they screwed the tooth back down I could feel that as well. Not truly painful but very uncomfortable. They removed the crown and put the healing seal back on again. My oral surgeon did a torque test and it read 50 inch pounds and he said that what was really good. While he did the torque test I felt it and it hurt in both directions but the implant screw wasn’t backing out. What could be wrong with this implant? Is this a titanium rejection? No other symptoms. I am afraid it is going to have to come out. I can take my finger and tap on the side of the crown (When the crown was on) and I can tap on the screw with the crown off the implant and there is tenderness. I don’t feel tenderness deep in the jaw. It just seems to be somewhere mid screw on up. There is also side to side major discomfort (not pain) I did not have any infection after the implant but I did have an infection under my tooth prior to the second and after the second root canal from the fracture. I could tap on my pre implant crown with a ballpoint pen and have the same sensation that I am having now from the dental implant crown on or off. It is not painful but it is the same discomfort. I would love your feedback. I did have plenty of bone and did not have to have a bone graft or stem cell bone material added. I am a male aged 50 with healthy gums and overall in good health.
I am going to ask my doc to run a titanium allergy test, ensure my bone density is good and I suppose they will put a bigger screw in next time. I was not told to eat soft food for 3-4 months.
I was eating normal food in a few days but chewed on the opposite side. I would say in 4 weeks I was eating normally. I would say I need to err on safety and have soft food for 3 months.
Hello Daryl: I really do not think this is a titanium or allergy issue. This may be an issue of lack of healing/integration of the bone against the implant. I say this because although the surgeon did a toque test and it seemed fine at “50” you should have not had the slightest feeling. I unfortunately have experienced the same thing when tightening an abutment or testing an implant. If there is pain, the implant is not fully integrated. Sometimes giving the implant a little more time is all that is needed. Sometimes the only thing that can be done is to remove the implant and start again….because what can occur iS some soft tissue ingropwth against the implant, and this soft tissue is what is preventing the bone from growing against he implant.The fact that you feel it also when you tap the crown is also indicative of this, although it could just be an abutment problem. However, because you also felt it at the torque test makes me think the issue is at the implant level.the best you can do is try to avoid eating on it for now to see if time will allow more bone growth/density in the area. Time will tell…sorry I can’t be more definitive at this time. Sincerely, Dr Balogh
Dr. Balogh,
I have two implants installed in my upper part of the right side of the mouth. However, I have been experiencing severe pain on the left side of my mouth, jaw, ear. X-rays, CT-scan do not show anything wrong and as dentist said it is not a typical case. Another words, my dentist(s) are not very helpful. I think that this is something to do with nerve, because I have strong sensitivity toward cold, difficulties to eat and swallow. Is there is any way to determine whether it is something to do with bone crafting? With incorrect placing of implants and etc? What test(s) can be done to determine what wrong with implants? Thank you
Hello Natalie: I agree that your symptoms are not normal or common. Without other symptoms, such as swelling, odours, drainage, sinus congestion etc it does not seem as though the symptoms are infection based. And apparently the ct didnt’ show anything also seems to confirm that it is not infection. Without seeing the clinical or radiographical findings it is impossible to comment on the implant placement, but in my experience and based on the anatomy of the area I would say nerve issues as a direct result of the implants are unlikely. How quickly did th symptoms develop. was it right after surgery or was it weeks later? If soon after the surgery it may be TMJ related due to opening wide for an extended period of time. fi TMJ. you can try heat, massage and antiinflammatories such as Advil, Motrin. If there is any relief from these then I would say there id defnintiley a TMJ/TMD component. Hopefully this helps. Sncerely,vDr Balogh
I just extractions if upper teeth last Monday had implants placed with done in one process (6 implants). Hybrid Placement was this past Wednesday. When screwing in, it was very painful on upper right but left side is fine. Very swollen also. On antibiotic and 800 mg ibuprofen for pain. I went back to my dentist
yesterday and he said what I’m experiencing is not unusual. There has been no
improvement and while I can’t predict, I can’t anticipate any positive change. Will have another follow up
on Monday. Anything else I should be aware of. Thanks
Hello EJ: It sounds as if when the teeth were placed the left side fit passively with the implants, but one of the implants on the right side may not be 100% passive and causing some pressure…since the implants were just placed this should subside fairly quickly and all the bone will remodel to the passive implant position. The other possibility is there was some pinching of the gum tissue as the teeth were inserted, however this usually subsides within hours of placement. By now this should have all resolved…my apologies for the late response!
Sincerely,
Dr balogh
Dr. Balogh
I just had a deep cleaning and was mentioned that my gums around my implant are a little inflamed. They did a 3d cat scan and noticed some bone loss around the area where my implant was placed. The implant has been placed for about 2 years now. There is no pain or movement of the implant. Also I do not bleed when I brush or floss that area. But they suggested I see my original oral surgeon. I’m worried it’s something serious. Any thoughts? Thank you
Hello Mike;
If there is some inflammation it is suggestive of bacteria/plaque collecting around the gum line and possibly below the gums. With bone loss some f the implant threads may not be covered by bone, and if so, this will be an area where bacteria can collect and be difficult to keep under control. One suggestion is to use a water pick and use hot salt water to flush out the area. Brushing and flossing does not clean very well under the gums…generally less that 2mm…so the water pick will be much more effective. Surgery and gum grafting may be suggested as a treatment, but my suggestion would be to try the water pick first to see if you get any improvement.
Sincerely
dr Balogh
Hi Dr. Balogh,
I recently had an implant placed on #30 by my oral surgeon 3 weeks ago. We used xenograft during placement due to minimal bone loss on the buccal side. We use PRF and integrate the bone into the PRF during the separation process in the centrifuge. Since placement, I’ve had nothing but trouble. 3days after placement i was in extreme pain. They went in and discovered the bone and some of my tissue had started to turn green on the underside of the implant location, not at the top. They removed what infection they could get to and put me on antibiotics. I went almost a week before having the same pain again. Not even Percocet was killing the pain. They went in again under GA this time, to be more thorough, and found the rest of the bone and some unknown material. Cleaned it out. Implant is still good and immobile. However, it’s been almost a week again and I’m still having pain. Under the jaw, near the lower ear, and trouble swallowing (it’s painful to swallow). When I’m not on meds, i can’t handle the aching. It’s as if I’m bending over and the blood is rushing constantly and hurts all the way to my collar bone. My surgeons say there’s nothing they see wrong. I shouldn’t be in pain. What could possibly be happening? Everything looks fine on exam, but pain control is an issue. I can’t take ibuprofen. Only Tylenol.
Hello Valerie:
It is hard to know what is happening going only by your history. One possibility that would create the pain is if the implant was placed with a lot of torque and the bone happened to be very dense, it could create some initial pain lasting for several weeks. However not sure what the unknown material would have been without seeing it and possibly sending out a specimen for diagnosis. I am sorry that it has taken this long to reply…I would expect that by now the pain has gone and the site has begun to heal or your dentist may have discovered the implant was now loose and had to bet removed.
Sincerely,
Dr Balogh
Hello Dr. Balogh,
I am 57, female. I have had 2 upper left implants (14,15) for about 4 years. I’ve been to an oral surgeon to ask about the health of my implants. He isn’t the original surgeon who did the work but a colleague. He told me everything looked fine. The implants are solid in bone. Below them is a space though with less than optimal bone, closer to the gum line allowing some pooling of saliva and food. He said it wouldn’t be advisable to mess with it and try to add more bone because it could disturb the implants and cause more bone loss. Good results would not be guaranteed.
My symptoms are I have thickness in the left sinus. I have had a mild runny nose on the left side sometimes. I been having this thick sinus sensation on the left for the last 4 months. Recently I got the flu and developed a sinus infection. It feels like the right sinus has no problems compared to the left and everything should have cleared up in the left but it’s inflamed. I don’t have pain. There can be a funky smell on the brush when using interdental brush to clean the site. I waterpik lightly rinse every night.
Complicating this, I have a severe TMJ problem. After many failed treatments, I have been helped seeing a TMJ dentist I am going toward full mouth reconstruction to create a functional bite as I don’t have one right now due to changes in the jaw. My jaw joints have healed but in CT do not look like the norm. I wear an appliance to eat and to create support. I really don’t need to be having problems with my implants and wonder if I had to get them out would a partial work? Like my mom? Seems like it might be healthier for my sinus.
I don’t see it as normal to live with sinus problems over the longterm.
Thanks for your opinion!
Ellen Golden
Hello Ellen: You brought up a number of issues, and I believe many of them are not necessarily related. From your description of the space around the implants I agree with your surgeon who said it would not e very predictable and probably not very successful. You may want to see if a new crown(s) can be made to close up some of the spaces and reduce food collection.
Regarding the sinus you may need to see an ENT specialist to look at your suite with either a scope or ct scan or both. It may be that your sinus issues are not related to your implants. Unless there is some serious problem with your implants, I would not recommend removing them to replace them with a partial. Partials also collect food and can cause issues with the natural teeth unless they are removed and cleaned after every meal/snack.
RE your water pick….that is a good thing to use…if you are not doing so I would;d recommend using hot slat water in your water pick…1.2 teaspoon salt in 600ml…the salt is antibacterial and will reduce the bacteria and smell.
lastly it may be that you do have some bite and tmp issues that may need the hep of aj prosthodontist or someone skilled in tmj/full mouth reconstruction.,
Hope this helps
Sincerely
dr balogh
Dear Dr. Balogh,
Thank you for your article and great explanation of the implants issues. I have some questions that I couldn’t find answers.
I recently broke my tooth with the crown, so there is only a root has left. My root’s channels were cleaned and sealed about 15 years ago. I wanted to save my tooth by installing posts into existing roots and build a crown on them, but my dentist does not recommend that as it won’t last very long. He recommended to instal an implant. However I’ve heard some concerns regarding a bone tissue that it may become thinner around the installed implant because there is no tooth anymore, which will lead to an implant failure.
I also have one missing tooth at another location for a very long time, so the bone is thin there and will require grafting if I want to install an implant. I’ve heard that there is a risk of cancer development due to that procedure.
I’ve tried to look for some researches or statistical data regarding those questions, unfortunately I was not lucky.
Could you please tell the possibility of these events and if you could recommend to read some literature that could help me in my decision?
I appreciate your any response.
Sincerely,
Natalia
Hello Natalia: I feel both of your concerns are unfounded. Placing an implant does not cause the bone to become thinner. Having an implant in place will stimulate the bone and allow it to be maintained and in many cases the density of the surrounding bone will increase. The exception is if the forces on the tooth/implant is excessive…in those cases bone will be overstressed and the bone around the implant will indeed be lost. However this can be minimized by placing an appropriate sized implant, making sure there is adequate bone volume, number of implants and adjusting the bite on the new tooth/implant.
Regarding bone grafting…I have yet to see any studies or articles, published or unpublished, linking cancer to bone grafting procedures. I have had bone grafting to three different sites in my own mouth and that thought never entered my mind.
sincerley
Dr Balogh
Hi Dr. Balogh-
I had a bridge fail due to fracture and had to have the. Ridge sawed off, tooth pulled and bone graft. Almost time to get the implant done. Reading through the comments. I am terrified of the implant failing and also scared because I have suffered from multiple chemical sensitivity in the past and wondering about titanium being a problem for me. Have you had patients with issues due to sentivity to materials? I wonder how much of the failure rate is due to this. Worried about systemic health problems. Do you have any experience with zirconium?
Hello Carol:
I have had many patients with multiple chemical and metal sensitivities, but yet to see anyone with a sensitivity to titanium. if you have any doubt or worries you can get tested to (www.cliffordlabs.com) find out if your body reacts to titanium as well as all the other dental materials. Zirconium is an excellent choice if you still have concerns. Implants are a wonderful solution for missing teeth…and although we do see some issues and even failures with implants it is significant lay less than we see with natural teeth, and the causes are not related to the material as opposed to other factors such as bacteria, bone volume/denstity/ treatment planning, hygiene etc.
Sincerely
dr balogh
I am allergic to titanium implants. I get zirconia implants. They r just as good!
Dear Dr. Balogh,
I have my number 3 extracted and bone grafting at the same time on August 29. On day 9 I felt bad smell from the site and stuffy nose at the same time. My dentist asked me stop amoxicillin and switched me to Biaxin. The stuffy nose was under control. Eventually he removed stitches on day 14, he found out the gum did not grow to cover the site. Some bone particles just scattered, embedded on the surface. It remained the same for next 8 weeks. During this 8 weeks, I felt discomfort on that area, and particles kept sticked out. Finally my dentist said it was too long, he needed to clean the surface and re-stitch the wound. He removed about 3 mm of the top, put a layer of collagen and membrane and used 13 stitches to close the area. This happened on Nov 5. He said no antibiotics needed this time. Only rinse and Qtip with chlorhexidine. He removed the stitches 16 days later. Before he removed the stitches, I felt a kind of pain on the surface of the area: some stitches grew into my gum! I thought that was the reason why I felt pain?. After removal of the stitches, my dentist told me the gum closure was definitely better than last time. I also felt good for the first a couple of days. Then I felt very itchy on the surface for about a week and now I feel a kind of pain again. The surface is red instead of pink. I really don’t know what is going on. Is this a normaI healing process or this is a bad infection? Please help me! Thank you very much!
Hello Lisa: It sounds as if you may have had a version of a dry socket initially after the extraction. Dry socket is something we typically see when we extract a tooth and do not place a graft, but I have seen a similar situation even with a graft. The site does not clot, many particles are loose and exposed to the oral envrionment, there is pain and often a smell. Your dentist did the right thing by cleaning out the site. Difficult to say why the area is red instead of pink. itchiness can be a good sign that it is healing. Two possibilities….one is that the area is healing but very slowly…the second is that there is a granulation type of tissue forming in the area in which case the granulation may have to be cleaned out.
sincerely
dr balogh
Hello Dr. Peter Balogh:
I had an infected tooth (bottom center, right tooth) with a healthy sized abscess. When I saw the endo, he told me the tooth next to it was affected as well and I’d need two root canals. They were only able to do a root canal on the non-infected tooth (the other tooth was too calcified).
Gameplan was to extract the infected tooth, cut open the gums, place a membrane and bone graft into the gums and suture me back up – that occurred on Monday, 2/11. Last night (2/15) I was eating and a small piece of the membrane came out. My dentist is OOO for another week, however, his staff told me not to worry this can happen and is a sign of healing – I’m due to see him a week from this Tuesday. In speaking with another Oral Surgeon they also told me not to freak out. Is my bone graft doomed? Thank you!
Hello Charles:
Sorry I did not see your inquiry until now…weekends are about the only time I have to check my blog for questions. Today is the 24th…about 9 days since part of of your membrane became exposed. To calm any fears or anxieties, membranes can get exposed and it does not mean that the bone graft is lost. Of course it is generally preferred that membranes do not get exposed as once exposed some the volume of bone anticipated may be less. Nevertheless bone grafts are often “overbuilt” to allow for some shrinkage or loss, so my feeling is as long as the site does not become infected or inflamed it will be OK. Simply try to keep the site as clean as possible. And on the other hand with certain grafts, such as socket grafts following extractions, it is practically impossible to not have the membrane exposed…so in those cases we use a membrane designed specifically for that situation.
Hope this helps a little.
Sincerely,
Dr Balogh
Hi,
happy to have found this site as gthere are no anwers anywhere…
I had an upper molar (right, next after wisdom tooth) extracted and got an implant a month later. Dentist said everything looked good, the implant was in the exact place though there had not been much room. I never experienced any pain. Two weeks later I woke up with the implant on my tongue. I had followed instructions but do remember biting on an only half cooked piece of broccoli once. I had had the implant looked at a week before it fell out and was told it was healing fine. Now the dentist is reluctant to try again and wants to do a fixed bridge instead. I believe there should be no reason not to try another implant. He is talking of ” not enough bone” and wants to do some bone rgenerating procedure – my understanding is that bone loss would be a preexisting condition if I had not had a tooth in that place for a long time or had any health condition. So: in your point of view, could I give the implant another try? If yes, how long to wait? If no, why? I am 53 years old and very healthy. There was never any sign of infection.
The other question is an ethical one: I have paid for the implant, not for the intent of an implant – what is the dentist’s responsability inj this case?
Hello Hannah: My feeling is that you probably can still have an implant placed. One month of healing in a molar site is a little too soon in my opinion. Although it certainly is possible to place an implant after one month, the lack of bone density in the area, the number of roots on the natural tooth and other factors makes it more risky at one month. Your dentist is probably correct though that you will need some bone augmentation….this area tends to not only have poor bone density, but the volume, in particular height is often minimal as the socket heals. Without seeing your dental records it is impossible to say which approach is best…it may be possible to augment the bone and place the implant at the same time, however the safer procedure would be to build up the bone, wait for ~4-6 months and then place the implant. Regarding costs, every dentist will have their own philosophy/policy as how they deal with these situations in a manner that is fair and equitable to both the patient and the dentist. Here in BC it is against our licensing body guidelines to actually “guarantee” or promise results (and my understanding is in medical procedures, eg a hip replacement, if it fails the hospital/doctors still bill for any revisions/redos required); however as dentistry typically falls outside the medical system, I believe most dentists will take these situations into consideration….I myself would not charge for a replacement implant, however there is no “requirement” per se so it is difficult/impossible for me to speak on others behalf. It is often best to discuss these things openly before treatment is started. Best to speak to your dentist how you feel and come to a favourable solution for both of you.
Sincerely,
Dr Balogh
Thank you so much for your timely and lengthy reply. Tomorrow I have my appointment and will ask about a few topics you mentioned. I hope it is ok to get back to you afterwards if I still have questions?? Thanks a lot,
Hannah
yes of course
I had 4 implants put in my lower jaw December 12th. Had immediate denture made to wear while they heal. The edge of the teeth sit on top of the implant. Very painful. The dentist wouldn’t do anything about it. So I started seeing another dentist in a different location but same company. He made a different plate and I cant wear them either because they are so wide, to go over the implants. I look like I have something in my mouth all the way around because the gums on the denture stick out so far. And is painful to have my mouth stretched for a short amount of time. And the teeth are set in. (I can send you pictures) . My question here is, am I seeing the wrong dentist or can teeth be made so they don’t look and do what these are doing? I have a small mouth and the denture plate is hard to even get in my mouth. I am still in pain with the 2 back implants. The 2nd dentist says they look really good in the x-rays and it will just take a while to heal. He said to wait 8 to 10 months to let the implants adhere to the bone before he can attach the teeth. The first dentist who pulled my teeth and put the implants in was very rough. I had bruises that went from my mouth all the way down my throat and on my chest. Have pictures of that also. I was on the pain meds he prescribed to have the procedure done so I wasn’t fully aware of what he was actually doing. He said he has never seen anyone bruise and swell as bad as I did.
I don’t bruise easily. Then he stopped communicating with me at all so I got the second dentist. I am afraid that I am on the losing end of this. I don’t know what to do. Your opinion would be greatly appreciated.
Sincerely
Melinda
Hello Melinda:
There are lots of potential reasons for many of your concerns (ie bruising, small mouth, how the surgery was performed etc) so it is really difficult to say much without seeing more myself and knowing more about what exactly was done, and how things are now. I do have concerns that the back implants are painful because they should not be after even one week. It could be that the gums are sore to the dentures and not the implants themselves, but once again I cannot say for sure. You do want to make sure that both you and your dentist are communicating well and are open and honest in both your current condition, your prognosis and the potential end result. It is concerning that your first dentist stopped “communicating”. Although it sounds as if your current denture is not fitting well and not comfortable, your dentist should be aware if these things will be remedied with the final teeth….as long as the implants were placed in an appropriate position for the final teeth then the final teeth will be a big improvement.In the mean time you may want to ask your dentist to try to adjust the denture to make it more comfortable while you are waiting for the implants to heal.
Sincerely
Dr Balogh
Dr. Balogh,
I have received 6 implants over the course of the last 10 years. 2 on the bottom and 4 on the top. Shortly after each of 3 implants were in and healed, an adjacent tooth cracked, vertically, through to the root. Those cracked teeth had to be pulled and resulted in the 3 remaining implants. My dentist and oral surgeon say my cracked teeth were from grinding my teeth at night. I’m pretty sure that I don’t grind my teeth and my husband concurs. It always seemed suspicious to me that these cracks each happened within a month or two after an implant was placed right next to them. I mentioned this to my dentist and the oral surgeon who placed the posts and they just shrug it off. My bite has also changed a lot. My teeth no longer fit together as they should. I have told this to my dentist several times over the last 3 years with the same lack of response. My husband mentioned to me today that my front teeth are beginning to look “bucked”, which is something new in the 40 years we’ve been married. He wonders if I need braces. Obviously my bite is still changing. Another new thing is that I can barely floss the teeth on the upper left side of my mouth, the teeth are so crammed together. My real teeth were never like that. My mouth no longer feels like my own. I have no idea what to do about it. I’m hoping you may have some suggestions. Thank you for any help you can give me.
Hello Gail:
If you do clench or grind at night, you or your husband may not be aware of it as we do it for a very short period of time, seconds to less than 1-2 minutes at a time. The wear and possible crack lines in your teeth will be more accurate evidence of this. Second our tooth alignment/bite changes with time due to tooth wear and dental work.Which one is causing the greatest effect is impossible to say…you may consider consulting with a prosthodontist…they specialize in restoring entire jaws/bites and they may be able to give you more insight as to shy your teeth are shifting and more importantly what to do to stop and or reverse the problem.
Sincerely,
Dr Balogh
Hello Dr Balogh! So excited to have found your blog. In September of 2017 I had a root canal on #13. It ached for 8 months until I finally had it retreated in July of 2018. All was fine until about two weeks ago when I started feeling some sensitivity to pressure as well as a bit of discomfort in the gums.
I went to the endo who did a 3D x Ray. The results were pretty inconclusive. He said that I have curved roots and it was possible that he entire canals weren’t filled. He also said that there could be what looks to be a hairline fracture in the root but he couldn’t be certain. His recommendation was to have the tooth extracted and do an implant. There would be no need for a bone graft as the bone is good.
Do you recommend doing an extraction and start the implant on the same day? Or is it best to wait until the extraction site heals?
They scheduled the extraction for a few days from now and I just don’t know if this is the right route to take. How successful are implants on an otherwise healthy mouth?
Hello Sarah
As long as the bone volume is good it is possible to place the implant at this same time.
Sincerely,
Dr Balogh
Thanks so much! One more question. I went ahead with the extraction and implant. It’s been one week since and the area where the implant is feels fine however the gums are quite tender still at the extraction site. A little read and somewhat sensitive to the touch. Is this normal one week out? Dentist took an x ray and said implant looks great and gave me a prescription mouthwash to help the gums settle. Is this normal to still be feeling some gum sensitivity? Thanks so much!
Hello Sarah
It is not unusual to have little redness, inflammation dn tenderness one week following an implant or any dental surgery for that matter. However, it hauled be improving daily or every coupe of days and definitely should not be getting worse and should not be severe.
Sincerely
Dr Balogh
Hello, Dr. Balogh, I also have a question regarding implants. I’ve had two implants put in my lower jaw to replace two molars. I had the surgery last month and now I’m in the osseointegration phase. I have noticed that in case of one of the implants I can feel a little bump in the labial mandibular gingiva (had to google this to better explain, I hope it’s accurate) and in the case of the other implant the gingiva feels smooth. I assume this bump is the screw of the implant. It also hurts a little bit if I press it with my tongue. The dentist did mention that I lacked width in the bone but no bone grafting was done.
Is it possible that the implant wasn’t placed properly or is it normal for some people to feel this bump and I worry over nothing?
Thank you very much!
Hello Eve:
It is really hard to say if this is a problem…sicne it is only one month it is still early in the healing phase. Certainly let you dentist know…it could simply be that the tissue is is thin…if there is no swelling, pain otherwise, infection etc then it may be OK. Sorry can’t give you more insight
Sincerely,
Dr Balogh
I’ve had three teeth (next to upper back molar) successfully implanted about 15 years ago. All was fine until about 6 months ago when I noticed discomfort when pressing my cheek next to my mouth. x-rays showed bone loss and a deep pocket. I recently saw my dentist who did a deep cleaning + bleach treatment. I have been seeing a hygienist every 6 months and keep my teeth spotlessly clean. However, neither I nor the hygienist have ever been able to get floss inside the 3 implanted teeth to clean the area. Yesterday the oral surgeon who inserted the implants along with a bone graft for the middle tooth did a deep curettage by opening the gum and removing granulated tissue. He is a very competent surgeon with a good reputation but doesn’t provide much explanation about the potential causes for this possible failure of the middle implant. He just says to keep it real clean and I may be able to save the middle implant. Can you share your thoughts? Does bleach do anything to kill bacteria in the long run?
Hello Marta
I feel diluted bleach solutions will kill the bacteria, change the environment and stop and potentially even reverse the bone loss. However you probably have a deep pocket in the area so the only way to use it effectively is with a water pick….rinsing will not be adequate. the other treatment to consider is ti find someone in your area who uses a periclase and can perform LANAP procedures…this is a laser technique that kills the bacteria and can be successful in giving the body a chance to regenerate the bone.
Sincerely,
Dr Balogh
Hi Dr,
I have a question regarding the insertion of dental implant. Would it overtime affect the brain due to reaction of titanium ions. If the implant is placed on the second back molar.
Hello Aaron
As far as I am aware, I have not seen any studies or evidence to indicate titanium ions are released causing harm….keep in mind there ore other sources of titanium such as cosmetics, sun tan lotions and foods etc that probably provide a greater body burden of titanium than an implant.
Sincerely
Dr Balogh
Hello Doc, thank you for doing all that you do.. I have 3 implants on bottom to secure my bottom dentures and they slip up and down. My dentist says that’s normal… I always have to take my teeth out to clean after I eat anything because good is all under my dentures.. he said that was normal as well.. I’m not as sure and need you, if you would, please tell me if it’s alright or not.. Sincerely, Yvette
Hello Yvette
Unfortunately with lower dentures there is always a bit of food that can and will collect underneath. It partly depends on the number of implants and whether they are splinted with a bar. The greater number of implants and the use of a bar allows your dentist to make the =denture more solid with less movement. However even the most sale lower denture will collect some food because the floor of the mouth moves ups and down with swallowing, eating and talking and gravity pulls the food down, so no matter what is done there will always be some plaque or food that collects. The best we can do is to make it as secure as possible without making the denture so rigid that it overload the implants and causes bone loss…that would be much worse.
Sincerely
Dr Balogh
Hi Dr. Peter,
I have a complicated question.
As a kid I damaged my front two upper teeth and they did root canal, posts and pfm crowns. Had them for many years until gums got inflamed in that areas and they pretty much had to be extracted.
I consulted with two oral surgeons and finally went with one who is very experienced and also does jaw, mouth surgeries.
At the consultation he said I had enough bone but if any was needed he would do it on surgery day. He said to remove roots and let area heal before placing the implants.
So everything went fine although after implants were placed I did notice my papilla gum in the middle was gone and one of the implants was placed deeper than the other. Still I generally trust professionals so didn’t say anything.
Day of crowns came and my dentist did mention one implant is deep so he had to numb my gum in order to put the crown.
Now the crown is weird, splinted (both crowns joined) with a gum colored bit in the middle where the papilla would be. The crown(s) feel really heavy kinda weird and I have had crowns there for many years. I feel the crowns are too bulky on the inside side where they are splinted. They are screw retained btw. I don’t like this at all, even my flipper felt better and lighter if that makes sense.
Is this the fault of the surgeon for not planning the gum contour properly and should vertical bone craft done prior? According the to the test my implants got integrated perfectly so how I fee these crowns, I hate that they are splinted and can the gum be fixed or does the implant have to come out and redone after graft? Is that even possible and would it cause more damage?
Thanks
Hello Gene:
First, the feel of your crowns is probably due to the size, shape and/or bite…these should be relatively easy to fix but may take some time/investigation by your dentist to truly figure out what it is about the crowns that feel odd. It should not make a difference whether they are screw retained or cemented crowns.
Regarding the loss of papilla…without seeing your situation it is difficult to say, however as a general rule once the papilla or tissue is lost it is much more difficult to recreate it. And now that you have the implants in place, doing a graft procedure to recreate more gums or bone can be very difficult if not impossible. It is always easier to do before the implants are in place because bone grows from apposition of nearby bone, and when and implant is in place there is less bone nearby and also less blood supply to any graft material.Whenever we place two implants side by side it can be very tricky to maintain the papilla and bone levels so that no obvious eshtetic change is visible in the before and after situation. In some cases tissue change is inevitable and when out it is I make sure to explain the potential outcome in advance…in other cases it happens despite our best efforts or even when we truly do not expect any tissue change…so I cannot say that it was anyones “fault” per se due to technique/procedure.
Before you have the implants removed or any corrective gum/bone treatment I recommend consulting with a periodontist to see if the area can be improved…removing the implant could make things worse.
Sincerely.
Dr Balogh
Hi Dr Balogh,
Thank you so much for the detailed reply.
I am more disappointed that my expectations were not set properly. There was no talk about gums, tissue absorsion etc at all. And as you say it is now too late to do much. Furthers my belief that most of dentists I have met throughout my life have done things worst for me and it’s hard for me to trust them and find someone who really cares and not trying to push me out the door as soon as they get paid.
I do now have another more pressing issue that developed as I was writing my earlier post. A day after the crowns placement I can feel my natural tooth next to the implant (has no restorations and is in very good shape) moves slightly. I noticed it when I was eating then I could move it with my fingers back and forth. I would describe it as slight movement but definitely not normal considering none of my other teeth do this. There’s no pain or any inflammation. I could not sleep because I was so worried. My dentist checked it out and says it’s normal, he did x rays and said it’s fine. I mean I trust him to some degree but at the same time I am not crazy, that tooth is mobile for sure, was not like that before and no other teeth do this. What could it be? I mean, obviously you don’t have a crystal ball so my question is probably who should I see to have this thoroughly checked?
Thanks for taking your time to reply.
Hello Gene:
Try placing your finger on the tooth and then closing on your back teeth, tapping moderately hard, then then grinding/sliding back and forth, left to right and front to back. You should not feel any “excessive” vibration or movement of the tooth…if so then it could be that your bite has changed slightly and now this tooth is being moved by your bite (we call this traumatic occlusion). the simple solution is to verify the situation and do a minor bite adjustment, after which the tooth should tighten up. Alternatively we have to look at the bone levels and any inflammation of the tissues….but you’re dentist already stated that these were OK. Wish I could suggest more…a this point it does not sound like a serious issue so want you to feel optimistic, however it is wise to be aware of all possibilities.
Sincerely
Dr Balogh
Hello Gene
It may be that your bite has changed slightly and you are now hitting the tooth heavily (traumatic occlusion/premature contact). A simple test is to place your finger on the tooth and then bite on your back teeth, tapping moderately, and then moving side to side and front to back. If you feel vibration in your tooth the bite may be off. A simple solution is to verify, identify and then do a bite adjustment. Your dentist has said there is no infection, inflammation on that tooth so I have to assume he/she is correct and the bite is the first thing that needs to be checked and ruled out.
Sincerely,
Dr Balogh
Hello Gene
It may be that your bite has changed slightly and you are now hitting the tooth heavily (traumatic occlusion/premature contact). A simple test is to place your finger on the tooth and then bite on your back teeth, tapping moderately, and then moving side to side and front to back. If you feel vibration in your tooth the bite may be off. A simple solution is to verify, identify and then do a bite adjustment. Your dentist has said there is no infection, inflammation on that tooth so I have to assume he/she is correct and the bite is the first thing that needs to be checked and ruled out.
Sincerely,
Dr Balogh
I had a dental implant put in about about 35 years ago due to an accident I had several years earlier which completely broke my tooth in half. There was a root canal performed on it at the time of break. This is a front tooth. Recently I had bit into a harder candy than I realized and have had a lot of pain every since(about a week). My gum above this implant has always been dark but is now black colored in front and back as if it is bruised right above the tooth. The tooth does not appear to be loose in any way. When eating or pressure (even a tiny bit) causes pain and aching and throbbing. Why would this happen so many years later? Will it heal itself or does it need looked into?
Hello Heather:
Definitely get your implant checked…this seems unusual. It is possible that your implant was healed but the integration (how well fused to the bone) may have been marginal or may have changed over the years…if so then you may have dis-integrated the implant. Hard to say what else it could be without seeing an x ray, ct scan and clinical presentation
Sincerely,
Dr Balogh
Hi Dr. Balogh!
My wife has an implant for one of the lower center teeth. The metal abutment can be discerned through the translucent crown. After an almost two-year ordeal with required bone-grafts, we feel the dentist should have at least told us beforehand that this would be the case. The dentist says this was unavoidable due to the small tooth that was being replaced. The color of the new crown tooth was matched to the color of the adjacent tooth, however, it appears darker because of the visible shadow of the abutment.
With today’s technology, I feel it would have been possible to manufacture a tooth where the inner portion ( closest to the abutment ) would have an opaque material super imposed with the final material which would made the crown appear like a natural tooth.
Please tell us what can be done to correct this problem.
Thank You,
Michael Sanchez
Hello Michael;
I understand the problem as I have had the same situation happen with some of my patients. The solution is usually fairly simple…the crown and abutment needs to be sent back to the lab and the ceramist needs to opaque the metal abutment. Once opaqued the dark colour will no longer show through. At this point however, the dentist may have to replace the crown depending on whether it is removable or not.
Sincerely,
Dr Balogh
Thank you Dr. Balogh!
It’s been about 17 months now since the crown was put in — I do not believe it is removable. I am all for asking the dentist to replace the crown however, my wife may be hesitant to ask the dentist to replace it because of the elapsed time.
Michael
Hello Dr. Balogh,
Background:
I had one dental implant (tooth #13) inserted on 7/11/2018. Tooth extraction, bone graft, GTR and implant were performed at the same time.
After implant, I had referred pain in left side – implant area pain radiating from nose to head to neck, with ear burning, jaw pain, heavy eyes and blurred vision, lip numb/tingling, and developed white tongue and low fever. The redness/swelling spread to tooth #14. Noticed gum recession on #12. My implant doctor said I was having sinus issues and prescribed: Amoxicillin and Clavulanate Potassium tables 875mg/125mg, and Flonase, Sudafed. He thought the pain was from tooth #14 because he transplanted gum from the back of #14 tooth to fill my implant tooth #13.
40 days after the implant, I had severe palate pain especially when I talked lasting for 20 days. Since that time, I saw 10+ implant specialists, a radiation specialist and a ENT doctor, I did CBCT twice and a Nasal Endoscopy. Two of the implant doctors suggested removing the implant after looking at the CBAT. I was told my implant is too close to the inside edge, hence the pressure and pain on my palate. Also, I was told the angle is not quite right compared to my bone (or other teeth) direction. One of the implant specialists mentioned that the referred pain might be the nerve of #13 that is connected to #14 or perhaps it wasn’t cleaned 100% during the extraction. All other implant doctors that I saw suggested that I go back to my implant doctor and ask him to open the area, if it was in good condition, and perform a healing cup or take the implant out. Of course, my implant doctor did the healing cup on 1/16/2019, and performed a torque test (35NCM, my implant is Straumann).
Current status:
My implant dr told me I can do crown now. However, I still see a white dot underneath the implant gum–my doctor said it’s bone graft. Gum around #13 and #14 are red, instead of pink.
When I press the implant healing cup, I have headache around my left temple and forehead.
When I eat, I feel sore from left ear to my left jaw, but not always.
Sometimes I feel pain around the back of my neck and head on the left side, but not always.
Should I remove my implant now? If so, will these symptoms go away after removing the implant? Or is the damage and symptoms permanent?
I would appreciate your thoughts. Thanks in advance!
Hello Jane
It sounds like you had some inflammation/infection developing in your sinus following surgery…your doc did all the right things to mitigate any further complications.
the white spot is very likely a piece of graft material…and if so it is not a problem and may even come to the surface and fall out
the redness around the #13 and 14 could be inflammation (does the gum bleed??) or may be minimal keratinized tissue around the teeth….this may not be a problem provided the areas stays clean, healthy and there is no inflammation
Your pain after eating….have your bite checked. You had a tooth removed at the time of surgery. this may have changed your bite…even one tooth can do this if a persons bite is not ideal. Have your teeth checked for posterior interferences in excursions, and any contacts on incline planes when biting in centric. As dentists it seems this has not been taught or explained well enough as to how much these tiny contacts can affect ones bite/comfort/tmj etc.
Re why you have pain when passing on the healing collar is a mystery….especially when the cbct showed all is ok. Best to proceed with caution…I would consider having a final abutment made and then a temp crown, or the final crown but inserted ‘temporarily” so that the area can be assess in function….but before proceeding do have your bite checked.
Sincerely
Dr Balogh
Hi Dr Balogh
I had one implant near the back of my mouth, top jaw. Ever since the implant I’ve noticed some tenderness and sometimes pain in the gum around an adjacent tooth. After exercise I can sometimes feel it pulsating and there is occasional sharp pain when biting. Is it possible that there is some nerve damage? Thank you
hello Helen
it doesn’t sound like nerve damage but does sound like there is some inflammation or even possible infection going on…..definitley let your dentist know and have them check out the tooth for any problems.
sincerely
dr balogh
I’m not sure you can help me but here’s my situation I had a complete restoration of my teeth. I later had to have two implants done on the eyeteeth upper I have constant infection I’ve been on anabiotic‘s often on for about a year and a half one of the crowns finally fell off it was re-cemented however the infection is still there there’s constant pus now I’m going to a new dentist a periodontist and he would like to lift the gums on the eyetooth and the And the two surrounding teeth and try to find out why I’m having these infections if it’s that the bone and the implant are not right my concern is removing the gum and lifting it up is it going To cause me gum problems is this the best way to treat my problem I surgery is scheduled for next week and I’m really concerned if this is the right thing to do I could really use your input thank you
Hello Iris. My apologies I have anywhere from 20-30+ questions each week, and when away or working through the weekend I fall behind….I’m assuming yo already had something done, so this answer may be more of a hope to others that yourself directly.
It probably is necessary to truly see what is going on by looking under the gums…one possibility is cement or debris under the gum. A ct scan beforehand can be helpful but even then it may not show cement. Beyond surgery,treateing the area with a periolase is an alternative solution….but even in some of those cases one still ends up having to explore the area surgically
sincerely
dr balogh
Dear Dr. Balogh,
I had my 3 implants done by a specialist but I don’t think he showed me if he places bone graft as a result; I only told him to place healing cap and then I will be heading to a dentistry dentist who will be placing 3 crowns in my mouth. I just want to know if I can find out if the bone graft is placed in my mouth through an x ray? Please let me know.
Hello Annie
the only way to see the graft on an X-ray is within 1-2 months of the procedure….and even then it may not show up on a traditional x ray…a ct scan would more likely show the prescence of graft material.
sincerely
dr balogh
I just returned from my 2nd appointment 6 months after the surgery. When the dentist said “OOPS! This is terrible,” I nearly dropped dead. He finally told me his number-machine-thingy was out of battery strength. I felt I’d returned from a war zone- twisting, jabbing, pulling and yanking… And I noticed he repaired the adjacent teeth somewhat because they looked a little different. Is this a typical appointment? Thanks. I’m still recovering from that ordeal
Hi Ellen:It is really hard to comment if what you had was typical since I don’t know what was being done. Certainly the comment was unfortunate as those things can easily be taken out of context by a patient who is passively sitting there listening but often cannot respond or question
sincerely
Dr Balogh
Reviewing yesterday, before I left, the dentist said the new image he took showed everything to be okay. But I am still worried and skeptical and dread the next appointment in 2 weeks.
Hello Ellen: At this point I’d say trust in what you have been told, particularly if everything seems ok to your dentist
Sincerely
dr Balogh
I did the first part of the implant and everything was going good. Took stitches out. And three weeks later you can see part of the screw. What happens now. Has this failed or can I still continue?
Hi Victoria
It has not failed…sometimes the gums shrink during healing…you can still continue
sincerely
dr balogh
Dear Dr. Balogh, I am 70, years old. I got my implants Aug.20, 2018. I am still in my temporaries. The bottom is fine. Although my chin is still numb and my lip feels weird. But the fit is ok. The uppers are not compfortable. They seem to be too tight in the middle. The sides are fine. It makes my nose feel numb sometimes. Will it be better with my permanent teeth or will I just have to live with this .
Hello Beverly
It is hard to say why you feel tightness in the upper front…definitely tell your dentist…ideally it would be best tomato changes to the temporaries first and get them 100% comfortable…otherwise if there is something in the fit/design of the teeth that is causing this then there is the chance the final ones may not be any better.
Sincerely
Dr Balogh
Hello!
Yesterday I had my crown fit and placed over implant . Dentist said it was a tight fit but nothing unexpected. Last night and today am experiencing pain in the adjacent tooth area when biting down . Is this normal sensitivity ? Will it go away on its own as the real tooth may shift gradually to accommodate the implant? Implant does fit right up against the side of the incisor-can’t even get floss thru it.
Thank you in advance for your answer!
Hello Lorraine:
It sounds like the contact was very tight, causing the adjacent tooth to move. This will make the tooth sore…often only temporary, but if it persists or you continue to have trouble flossing the area then the crown will need a minor adjustment
sincerely
Dr Balogh
Thank you for addressing everyone’s issues, Dr. Balogh, I cannot find any similar issue to what I have going on though. I had 2 extractions on my bottom left molars (the two in front of my bottom left wisdom tooth) and had 2 implants and crowns installed 5 years ago. The crown immediately in front of the wisdom tooth falls off every few months, and my dentist reseats it. My issue is the other implant (2 molars in from the wisdom tooth) where the implant post SHEARED OFF. I have half of the post embedded in my jaw, with a tiny amount of post sticking up through my gum line. My dentist has never seen an implant post snap in half in his 35+ years of dental practice. I do not have $15,000 to redo both implants (that was the original cost 5 years ago) but my biggest issue and concern is that 6 days ago the entire left side of my head, face, lip, and inside my mouth went completely numb, almost paralyzed. A trip to the ER for a CT Scan showed no sign of a stroke or aneurism, so I am wondering if the numbness may be due to an allergic reaction to the metal in the implant post? At this point, I just want the implants removed, as I have had nothing but issues every day with these implants since the day they were installed. Do you think it is possible that I have nerve damage from a reaction to the metal posts? And if so, will removing them from my body give me the feeling back in my face? I cannot function like this, and am scared to death of permanent nerve damage that may have been caused by the implants. Your advice would be greatly appreciated, thank you for responding to everyone’s questions!
Hello Dee:
It would be very important to accurately “map out” the area of the face that has been affected…that will determine which nerve has been affected and then that could also help determine the cause. I don’t think it is a result of nerve damage from a metal reaction/allergy. There may however be some infection around the failed implants which is causing the problem…but the mapping will determine if that is the likely cause (inferior alveolar nerve). If the numbness extends to your face on the exterior, it is more likely the facial nerve or something else…in which case I doubt it is related to the implants.
Although rare, I have seen implants fracture. However it is almost always with someone who is a very heavy clencher or grinder (bruxism). IF I am correct this could also contribute to your numbness. In which case controlling and mitigating the clenching habits will help with the numbness.
Sincerely,
Dr Balogh
Hi. My tooth # 30 (lower left) was extracted last year in a legitimate clinic in Canada. My dentist told me to let it heal for 4 months, so I did. Everything was fine. Then about 6 months ago, I got a dental implant there with bone grafting. (I think it’s bovine.) I got the “nail” (the lower part/implant) planted into my gum with bone grafting. I still haven’t got the upper part (the “tooth”/crown) on because my dentist told me to let it heel for 5 months. My dentist told me that my face would be swollen for 3-4 days after the surgery, and it did. Then the swell reduced and everything went back to normal except one thing. There is still a little bulge on my left cheek that won’t go away and it’s been about 6 months since the implant surgery. The bulge is not obvious. Strangers and people who don’t know me very well don’t notice it, but I myself and my parents can definitely see it. It’s a little bulge but it’s there. My left cheek’s not the same as before the implant surgery. It doesn’t hurt no matter how I touch it. Can someone explain to me what’s wrong with my left cheek? Why doesn’t the little bulge go away? Will it disappear eventually? What caused it to remain there? Thank you very much.
Hello Jack
It is difficult to say without seeing the site myself. However I assume the bulge is actually on the side of the jaw bone as opposed to being in the soft tissue of the cheek. If so then it probably is a result of the bone grafting…the bone may have been overbuilt (which is common) as the bone will often shrink. If I am correct and the bone does not shrink it is very easy to reduce the excess bone. However if it is not obvious, unless it bothers you so much that you cannot take your mind off of it, I would leave it alone…with time the area will likely shrink although it may be a matter of 12-18 months
sincerely
dr balogh
Five months ago I had two zirconium implants with abutments put in to replace the previously removed top left molars. It went fine and I’ve had no pain or discomfort since. Then 10 days ago the zirconium crowns were finally placed on top of implants. I had some pain, discomfort and tightness during the procedure but the surgeon said it was normal and should go away the next day; he also adjusted the bite and shaved off some of the crowns as I complained they felt too big. Now it’s been 10 days and while the pain is mostly gone, the tightness, pressure and discomfort are the same or worse. The crowns definitely feel too big all around, not only too long (which interferes with bite) but also too thick. I’ll most likely go back for a follow up next week, but am not sure what to ask for. Is it normal to feel constant tightness/pressure with implant crowns? If not, what can be done short of removing them and making new ones (which I can’t afford). And, since it’s important to get the crowns right as you only get one shot, why haven’t temporaries been placed first? (it has only occurred to me now as this is one of the top oral surgeons at a Manhattan dental offices and I assumed he knew what he was doing).
Hello Al: I would say the tightness should not last beyond one day. Part of it sounds like your bite is high, which can be adjusted. The shape may feel big to your tongue…often that goes away as the tongue accommodate to having teeth in place again, however if it persists beyond 2- 3 weeks the shape of the crown could be reduced.
Are the teeth also tight to floss? if so then I would say the contact between the teeth is too tight and that can be adjusted even if they are cemented ( although not as easily if they could be removed). The other possibility is the shape of crowns near the gum tissue is such that it is impinging on the gum tissue excessively. If mild this is usually gone in 24 hours or less as mentioned above…however if it persists then either it will be a matter of waiting for the tissues to slowly modify (which could take months). Normally if there is any doubt about the fit the crowns can sometimes be placed with a temporary cement so that they can easily be removed and modified as needed.
Talk to your dentist about how they feel and where you sense the pressure. I am sure they will be able to determine the cause and rectify the issues.
sincerely
dr balogh
Hi Dr. balough, I’m 38 years old. I have four unit upper front teeth bridge between my two canines. It is failing and loose. Can I get an implant bridge? My dentist told me It will be difficult because I have class III malocclusion. I don’t want partial dentures. I had it for ten years and I don’t like it. Or a new bridge which will touch my canines. Am I a hopeless case?
Hello Jane: Your dentist is correct in that a class II bite will put more stress and strain on your upper front teeth. However that does not necessarily negate implants or a canine to canine bridge. However it will be important to wax up your teeth on a model and see how it will also look in the mouth from an esthetic and functional point of view, as well as available bone and strength of the remaining teeth. You are not a hopeless case…it just takes more care and planning, and possibly some small compromises.
sincerely
Dr balogh
Dear Dr. Balogh
I have recently had an implant (2nd from back lower molar) The tooth that was fitted is a little short on height leaving about a 1/2mm gap from the above tooth. I was told that it needs to be shorter to lessen impact of chewing but the gap seems too much and it often leaves food in the new tooth.
Is it normal to leave such a significant gap?
Kind Regards
David
Hello David
It is normal to have an implant crowns slightly light in contact…when we clench/chew teeth will depress ~25-30 microns, whereas an implant will only depress ~3-5 microns. Hence the light contact prevent the implant from being overloaded. However I personally do not feel the gap should be so big that one can feel a difference or that food gets stuck on the biting surface. Best ot speak to your dentist about it…they can probably unscrew the crown and have the lab add more porcelain to the biting surface.
Sincerely
dr balogh
I had 6 implants and 3 failed. I now have a feeling that something is protruding in my gum and a bit of pressure where another implant is. I assume this is also a
failure? Went to oral surgeon last week and he said the 3 remaining have integrated well and are ok. Why the feeling I am having? This whole ordeal has caused me a mass amount of anxiety.
It may be that the implant has integrated but there has been some minor bony change near the crest, just under the gum. So when you look you may be seeing the top of the implant…the only way to now for sure would be with a ct scan or opening the tissue to see how the bone is around the implant. However, if it is minor then your implant can still be very successful and useful, and if it is more than minor the area can often be grafted further as needed.
Sincerely
dr balogh
hi dr Balogh,
Im a dental biller in NY. Medicaid recently started covering some or very little implant coverage. Patient presented after two years with implants and wants Medicaid to cover implant crowns. He currently filed an appeal b/c surprise, surprise, the crowns were denied… so now he is in a court appeal and the court asked us to write a note why the crowns are now medically necessary. Are they truly necessary at this time or can he wait to have crowns put in. How long can he wait? What if he never puts crowns in? is there a chance of implant failure or micromovement?
I don’t think there is any worry about micromovement of the implants. In my opinion the necessity of the crowns would be for function and to prevent other natural teeth from tipping or over erupting into the empty space.And that may also depend on which areas have the the implants and how the overall bite/function is currently. By waiting there should be no harm to the implants per se, but if one waits too long then the other natural teeth may shift/overerupt
Hope this helps
Sincerely
dr balogh
Hello Dr.Balogh. I am looking at full mouth denture implants. Some have 2 posts per bridge and some 4 or even 6. My dentist is offering the 2 post full denture implant, which is more affordable. Is there an advantage of having more than 2 posts? Thanks for your time and effort.
Hello Marck
I may have misunderstood your question..but here goes…
One of the biggest contributors to failure of implants in the long term is underengineering….ie toot few implants for the number of teeth they support…this leads to over stressing the of the bone, bone loss and then potential loss of the implants. You can used two implants to help keep a denture from falling out, but not to support a full arch of teeth. Two implants are adequate to support a bridge involving 2-4 teeth provided the implants are adequate in size and position, the bone is adequate in density and the rest of the bite is satisfactory.
Hope this helps a little
Sincerely
Dr Balogh
Hi Dr Balogh, I had a failed root canal, …setup for an implant , but found infection in the extraction site…had the bone scraped out, long story short some 12 months later I have fused screw to the bone , but upon placement of the crown, pain seemed to increase …just recently crown removed on a trial a few days ago….to see if pain decreases…my question , my type of pain is a constant burning ache, followed by a occasional throbbing ache.. ( much like a nerve )…and it seems this throb, is increased with hot liquids, is this normal ?, or is there another possible area of cause ?…I cannot address the pain to any other specific tooth….as the throb, kinda feels bone based, ..at the moment I am just waiting a few weeks to see if it settles …. ut any ideas of the best wAy forwArd is much appreciated….
Cheers Shane
Hello Shane
It does seem odd that the symptoms began months after the implant was surgically placed. Although I would nt rule out the implant, my feeling is the teeth on both sides should be throughly assessed fro vitality and then a ct done of the area to see what if anything is going on around the implant
Sincerely
Dr Balogh